Vena Galeni Malformation



















Vein of Galen aneurysmal malformations (VGAMs), probably better termed as median prosencephalic arteriovenous fistulas, are uncommon intracranial anomalies that tend to present dramatically during early childhood with features of a left-to-right shunt and high-output cardiac failure.
Epidemiology
These malformations account for less than 1-2% of all intracranial vascular malformations but are the cause of 30% of cerebral vascular malformations presenting in the pediatric age group . It is also the most common antenatally-diagnosed intracranial vascular malformation. There may be an increased male predilection .
Clinical presentation
Increasingly the diagnosis is being made antenatally with third-trimester antenatal ultrasound. Presentation is often with high-output cardiac failure in the neonatal period, although low-flow aneurysms may remain undetected into adulthood. As much as 80% of cardiac output may shunt through the fistula. The presentation does, however, vary with the type of malformation, and different types present at different ages:
- neonate
- usually choroidal type
- high output cardiac failure
- cranial bruit
- infant
- usually mural type
- hydrocephalus may occur due to venous hypertension or aqueduct stenosis
- child
- usually mural type
- developmental delay
- hydrocephalus
Pathology
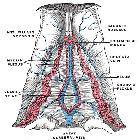
The anomaly is actually due to a cerebral arteriovenous fistula of the median prosencephalic vein (MPV) (a precursor of the vein of Galen) occurring at 6-11 weeks gestation and not a malformation (no nidus present). The MPV fails to regress and becomes aneurysmal. It drains via the straight sinus (present only in 50%) or a persistent falcine sinus, and the vein of Galen does not form.
Haemodynamically cerebral arteriovenous fistula involving vein of Galen can be subdivided into two groups:
- true VGAMs
- vein of Galen dilatation secondary to high flow parenchymal AVMs draining into this vessel
Classification
Malformations have been classified in a number of ways starting as early as 1960 when Litvak et al. recognized the need for a classification system in the region of the vein of Galen. Over the years, the most commonly used systems of classification are:
- according to clinical presentation (see above)
- Yasargil classification: types I to IV
- Lasjaunias classification: choroidal and mural types
Mortazavi et al. in 2013 proposed a new classification system (not validated) incorporating two important factors: heart failure and age.
Radiographic features
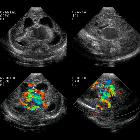
Antenatal ultrasound
With increased availability and quality of antenatal ultrasound, the diagnosis is increasingly made prior to delivery. Antenatal detection is however mostly reported late in pregnancy (3trimester).
The dilated median prosencephalic vein (MPV) appears as an anechoic structure in the midline posteriorly and demonstrates prominent flow on Doppler examination. Shunting may lead to complications such as hydrops fetalis or fetal cardiomegaly.
CT and MRI
Both CT and MRI can be used to delineate the malformation cross-sectionally.
CT angiography
CTA in neonates with high output cardiac failure is technically-challenging due to the small volumes of contrast and very rapid passage of contrast through the circulation.
MR angiography
The dilated feeding and draining vessels appear as flow-voids on T2. MRA may also be performed which would better delineate vascular anatomy.
Angiography
Angiography remains the gold standard in full characterization of the lesion. It enables to individually catheterize feeding vessels. Morphologically a spherical or ellipsoid varix may be visualized. Venous drainage is via the median prosencephalic vein (MPV), the straight sinus (if present) and then out via the transverse/sigmoid sinuses. By definition, there should be no drainage to other components of the deep venous system .
Treatment and prognosis
Prior to endovascular intervention, the prognosis was dismal, with 100% mortality without treatment and 90% mortality following surgical attempts .
Ideally, embolization is deferred until 6 months of age for choroidal VGAM and later for mural types, to allow the cavernous sinus to mature. If cardiac failure is refractory to medical management, embolization may be performed sooner.
Both venous and arterial embolization is possible, depending on the number of feeders, and controversy persists in regards to the optimal approach. Options include :
- arterial feeder and fistula occlusion
- transtorcular or transvenous embolization of the dilated vein
- complete or incomplete occlusion
Both coils and acrylic glue can be used in a single procedure or in staged approach .
Radiosurgery has been tried but is limited to patients who are not candidates for other treatment modalities .
Hydrocephalus is typically not shunted, as this may exacerbate cerebral ischemia by altering cerebral hemodynamics and due to the increased risk of intraventricular hemorrhage.
The prognosis is determined mainly by the presence or absence of cardiac failure. Thus choroidal types and those presenting in the neonatal period do poorly.
History and etymology
Vein of Galen malformations are named after Galen of Pergamon (gr. Γαληνός, also known as Aelius Galenus or Claudius Galenus) (AD 129-199), a Greek physician and philosopher in the Roman Empire .
Differential diagnosis
Once abnormal vessels are identified, there is usually little diagnostic uncertainty, with the only two entities to be considered being:
Siehe auch:
- Arteriovenöse Malformation
- Vena cerebri magna
- intrakranielle vaskuläre Malformationen
- lasjaunias classification
- intrakranielle arteriovenöse Malformationen
- zerebrale venöse Malformationen
und weiter:
- Hydrops fetalis
- obstetric curriculum
- abnormal ductus venosus waveforms
- cavum vergae cyst
- yasargil classification
- median prosencephalic vein
- fetal intra-cranial cystic lesions
- fetal cardiomegaly
- cerebral malformation
- persistierender Sinus falcinus
- fetal arachnoid cyst
- fetal arteriovenous malformations
- fetale Tumoren
- Klassifikation zerebraler vaskulärer Malformationen
- completely thrombosed aneurysm of the persistent, primitive prosencephalic vein of Markowski

 Assoziationen und Differentialdiagnosen zu Vena Galeni Malformation:
Assoziationen und Differentialdiagnosen zu Vena Galeni Malformation: