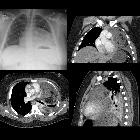
mediastinal teratoma




















Mediastinal teratomas are germ cell tumors located in the anterior mediastinum, representing the most common extra-gonadal germ cell tumors.
Epidemiology
They account for approximately 15% of anterior mediastinal masses in adults and approximately 25% of anterior mediastinal masses in children. They are by far the most common mediastinal germ cell tumor, accounting for 50-70% of such tumors .
The age of presentation is wide, but the typical presentation in adults is in the third or fourth decade (the 20s and 30s). In children below one year of age, immature teratomas are common (40%) and may be detected antenatally .
No particular gender predilection for mature teratomas has been identified (at most there is a slight female predilection). Immature teratomas, however, occur almost exclusively in males .
Clinical presentation
The majority of patients are asymptomatic, with the mediastinal mass discovered incidentally when the thorax is imaged for another reason . Masses that become symptomatic can do so in a variety of ways:
- mass effect
- respiratory distress (infants)
- respiratory failure
- superior mediastinal syndrome
- neck mass
- Horner syndrome
- endocrine function
- hormone production, e.g. beta-HCG, insulin
- rupture
- chest pain
- hemoptysis
- respiratory distress
- cardiac tamponade
- pleural effusions
Pathology
Mediastinal teratomas are germ cell tumors arising from ectopic pluripotent stem cells that failed to migrate from yolk endoderm to the gonad. By definition, they should contain elements from all three embryological layers: endoderm, mesoderm and ectoderm. Frequently, however, elements from only two layers are evident (see teratoma article).
A mediastinal dermoid cyst can be considered a variant of mature teratoma, predominantly formed by squamous epithelium and skin appendages (ectoderm and mesoderm respectively) .
Teratomas may either be:
- mature: well differentiated
- immature: poorly differentiated
- with malignant transformation
- mature teratoma with non-germ cell malignancy arising from one of the components
Because they originate from primitive cells, they have variable neoplastic potential. Generally, cystic lesions tend to be benign whereas solid lesions tend to be malignant; however the final diagnosis is made histologically.
Mature teratomas and most immature teratomas are benign tumors, but still, carry a risk of malignancy despite being indolent initially and require close clinical, serological, and radiological follow-up, or surgical excision. There is also a low incidence of malignant transformation of somatic cells (i.e. non-germ cell components) within these tumors, e.g. carcinoma, sarcoma, leukemia .
Location
Usually occurs within or near the thymus gland.
Associations
Mature teratomas have been associated with:
- Klinefelter syndrome (47, XXY)
Immature teratomas can be associated with:
- non-lymphocytic leukemia
- pleomorphic undifferentiated sarcoma
Radiographic features
The vast majority of mediastinal teratomas are located in the anterior mediastinum (80%), with most of the remainder involving multiple compartments (13-15%). Isolated posterior or middle mediastinal location is uncommon (2-8%) .
Mature teratoma
Mature teratomas, by their very nature, may contain a vast range of tissues and thus have variable imaging features. In general, they have the following features:
- well-demarcated, displacing rather than invading adjacent structures
- large: 3-25 cm
- usually cystic: 90%
- may be uni- or multiloculated
- septal/rim contrast enhancement
- variable attenuation, consistent with different tissues
- fat
- water density cystic spaces
- fat-fluid levels (specific)
- homogeneous soft-tissue density
- calcification: 26%
- identifiable teeth or bone is seen in up to 8% of cases
When rupture has occurred, the density of each component is less likely to be homogeneous, but rather each part of the teratoma is heterogeneous (i.e. the fat component is heterogeneous, as is the cystic component etc.) .
Immature
Immature teratomas are usually solid.
Plain radiograph
Appearances on chest radiography are usually indistinguishable from many of the other causes of an anterior mediastinal mass. Calcification may be visible.
CT
CT is the mainstay of diagnosis. The appearance will depend on the type of teratoma, and whether or not a cystic teratoma has ruptured. They are all however usually located in the anterior mediastinum.
Treatment and prognosis
Treatment depends on whether the teratoma is mature or immature. In the former, surgical resection is curative. In the later management depends on alpha-FP levels. If these are elevated then postoperative chemotherapy is usually employed .
Prognosis of mature teratomas is excellent as they are benign tumors. Pure immature teratomas also usually have an excellent prognosis, especially in childhood. In up to 30% of cases, however, immature teratomas have a malignant germ cell tumor component (most frequently yolk sac tumor), which result in frequent (25%) recurrence. Nonetheless, with adjuvant chemotherapy, a greater than 80% three-year survival can be achieved in children. Prognosis in adults is less favorable .
Potential complications include
- respiratory distress/failure: infants>adults
- hemorrhage
- pneumothorax
- fistula(e) formation: aorta, SVC, esophagus, bronchus
- rupture
- bronchus: trichoptysis is virtually pathognomonic
- pericardium: pericardial effusion and tamponade
- pleural cavity: pleural effusion
Differential diagnosis
On chest radiography, the differential is broad, and includes any cause of an anterior mediastinal mass:
On CT the differential is usually narrowed to tumors and depends on the morphology:
- mass containing fat
- heterogeneous soft tissue
- other germ cell tumors: mnemonic SECTE
- lymphoma
- thymic tumors
- predominantly cystic
Siehe auch:
- Bronchogene Zyste
- Teratom
- Tumoren des vorderen oberen Mediastinums
- Keimzelltumor
- Thymuslipom
- Thymuszyste
- mediastinale Keimzelltumoren
- nichtseminomatöser Keimzelltumor
- Tumoren des Thymus
- Merkspruch Keimzelltumoren
- SECTE
und weiter:

 Assoziationen und Differentialdiagnosen zu mediastinales Teratom:
Assoziationen und Differentialdiagnosen zu mediastinales Teratom:








