spinal ependymoma


















Spinal ependymomas are the most common spinal cord tumor overall, seen both in adult and pediatric population.
This article specifically relates to spinal cord ependymomas. For a discussion of intracranial ependymomas and for a general discussion of the pathology refer to the main article: ependymoma. Additionally, due to different imaging features and demographics, myxopapillary ependymomas are also discussed separately.
Epidemiology
Spinal ependymomas are the most common intramedullary neoplasm in adults, comprising 60% of all glial spinal cord tumors. They are the second most common intramedullary neoplasm in the pediatric population, representing 30% of pediatric intramedullary spinal neoplasms .
Peak incidence is in the fourth decade, with 39 years being the mean age at presentation. Males are more commonly affected than females.
There is an increased coincidence with neurofibromatosis type 2.
Clinical presentation
Clinical presentation is similar to that of other intramedullary spinal tumors, with pain, weakness, and sensory changes common.
The frequent presentation of sensory symptoms may be explained by the proximity of these centrally located tumors to the spinothalamic tracts. Dominant motor symptoms are commonly associated with very large ependymomas .
Pathology
Ependymomas arise from ependymal cells lining the central canal or cell rests along the filum. Six histological subtypes are recognized:
- cellular (the most common intramedullary type)
- papillary
- clear cell
- tanycytic
- myxopapillary
- virtually always located along the filum terminale with occasional extension into the conus medullaris
- discussed separately: see myxopapillary ependymomas
- melanotic (the least common type)
On histologic evaluation, uniform moderately hyperchromatic nuclei are typically observed. Perivascular pseudorosettes are the classical finding.
Using the WHO classification, almost all intramedullary ependymomas may be classified as grade II or sometimes III (anaplastic). Malignant types are rare.
This is in contrast to myxopapillary ependymomas which are grade I lesions.
Radiographic features
Ependymomas can occur anywhere along the spinal cord, however, the cervical cord is the most common site (44%). An additional 23% occur within the cervical cord and extend into the upper thoracic cord, and 26% occur in the thoracic cord alone .
Plain radiograph
Plain film features that may be seen with a spinal ependymoma include:
- scoliosis
- spinal canal widening
- vertebral body scalloping
- pedicle erosion
- laminar thinning
CT
CT may demonstrate:
- non-specific canal widening
- iso to slightly hyper-attenuating compared with normal spinal cord
- intense enhancement with iodinated contrast
- large lesions may cause scalloping of the posterior vertebral bodies and neural exit foraminal enlargement
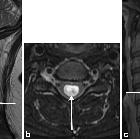
MRI
MRI is the modality of choice for evaluating suspected spinal cord tumors. Features include:
- widened spinal cord (as ependymomas arise from ependymal cells lining the central canal, they tend to occupy the central portion of the spinal cord and cause symmetric cord expansion)
- although unencapsulated, they are well-circumscribed
- tumoral cysts are present in 22%. Non-tumoral cysts are present in 62%
- syringohydromyelia occurs in 9-50% of cases
- in contrast to intracranial ependymomas, calcification is uncommon
- average length of four vertebral body segments
Typical signal characteristics:
- T1: most are isointense to hypointense; mixed-signal lesions are seen if cyst formation, tumor necrosis or hemorrhage has occurred
- T2: hyperintense
- peritumoural edema is seen in 60% of cases
- associated hemorrhage leads to the “cap sign” (a hypointense hemosiderin rim on T2 weighted images) in 20-33% of cases . The cap sign is suggestive of but not pathognomonic for ependymoma as it may also be seen in hemangioblastomas and paragangliomas
- T1 C+ (Gd): virtually all enhance strongly, somewhat inhomogeneously
Video tutorial
Treatment and prognosis
Most ependymomas are slow-growing. They tend to compress adjacent spinal cord tissue rather than infiltrate it, almost always leaving a cleavage plane between tumor and spinal cord tissue.
A complete curative excision may be achieved in approximately 50% of cases. In those patients, the 5-year survival rate is approximately 85%. In patients who are not able to achieve complete resection, the 5-year survival rate is approximately 57%. Recurrence is rare following complete excision.
Although metastatic spread is rare, the most common sites for metastases include the retroperitoneum, lymph nodes, and lungs .
Differential diagnosis
On MRI, the main differential diagnosis is an astrocytoma. Certain imaging features may help to differentiate between the two, which are covered in this article:
- astrocytoma
- most common spinal cord tumor in children
- eccentric location in the spinal canal
- ill-defined
- hemorrhage is uncommon
- patchy irregular contrast enhancement
- bone changes are infrequent
- involvement of the entire cord diameter and longer cord segments favors an astrocytoma (i.e., if an intramedullary neoplasm involves the total spinal cord, it is more likely to be an astrocytoma )
- spinal cavernous malformation
- no enhancement
- complete hemosiderin ring
Siehe auch:
- Aneurysmatische Knochenzyste
- Chordom
- Ependymom
- Riesenzelltumor
- Astrozytom
- spinale Schwannome
- Cauda equina Lipom
- spinal paraganglioma
- intradural spinal mass lesions - an approach
- spinales Ependymom des Filum terminale
- spinale kavernomatöse Malformationen
- Neoplasien der Cauda equina
- ependymoma vs astrocytoma of the spinal cord
- intramedulläres Ependymom
und weiter:
- Funikuläre Myelose
- neoplasms of the spinal canal
- spinal myxopapillary ependymoma
- spinales Hämangioblastom
- cap sign of spinal tumour
- spinales Astrozytom
- Tumoren der Kauda und des Filum terminale
- Lymphom des spinalen Myelons
- Spinal gangliogliomas
- primary spinal lymphoma
- solitärer fibröser Tumor des Rückenmarks
- haemosiderin cap sign
- malignant ependymoma
- myxopapilläres Ependymom des Sakrums
- zystisches Ependymom

 Assoziationen und Differentialdiagnosen zu spinales Ependymom:
Assoziationen und Differentialdiagnosen zu spinales Ependymom: