Thyroid-associated orbitopathy


















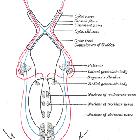
Thyroid-associated orbitopathy (or thyroid-associated ophthalmopathy) is the most common cause of proptosis in adults and is most frequently associated with Graves disease. On imaging, it is characterized by bilateral and symmetrical enlargement of the extraocular muscle bellies. The typical distribution is inferior rectus > medial rectus > superior rectus, with sparing of their tendinous insertions.
Epidemiology
The demographics of thyroid-associated orbitopathy reflects that of patients with thyroid disease and is, therefore, more frequently seen in women. Although Graves disease is the most common cause, Hashimoto thyroiditis has also been implicated. It may precede the onset of abnormal thyroid function, occur concurrently, or commence following its onset.
Clinical presentation
- lid retraction
- proptosis, with resultant chemosis and corneal dryness and ulceration
- optic nerve compression, potentially leading to blindness
- diplopia
- hypoglobus: uncommon
Pathology
Thyroid-associated orbitopathy is characterized by enlargement of the extraocular muscles as well as an increase in the orbital fat volume . While the exact mechanism is unknown, antibodies to thyroid-stimulating hormone (TSH) appear to cross-react with antigens in the orbit resulting in infiltration by activated T lymphocytes , with subsequent release of inflammatory mediators.
The muscles are infiltrated with inflammatory cells (lymphocytes, macrophages, plasma cells, and eosinophils), and increased mucopolysaccharide deposition. In long-standing cases, increased collagen deposition leads to fibrosis .
Involvement of the extraocular muscles in decreasing order of frequency:
- levator palpebrae superioris muscle
- inferior rectus muscle
- medial rectus muscle
- superior rectus muscle
- lateral rectus muscle
- oblique muscles
The order is captured by the mnemonic I'M SLOw, with the exception of the levator muscle .
An increase in orbital fat volume is a result of venous congestion from the compression of the superior ophthalmic vein by the enlarged muscles and/or intrinsic adipose inflammation.
Radiographic features
CT
Due to its widespread availability and rapid image acquisition, the diagnosis is often first made on CT. Intravenous contrast, although ideal, is not necessary, as the differing densities of orbital fat and muscle allow for adequate delineation of the orbital contents.
Findings include:
- exophthalmos
- the reference line for measurement of proptosis is the interzygomatic line (a line that connects the anterior edges of the zygomatic bones):
- the distance from this line to the posterior sclera is normally 9.9 +/- 1.7 mm
- the distance from this line to the anterior surface of the globe should be <23 mm
- a greater distance indicates exophthalmos
- extraocular muscle enlargement and fatty attenuation
- characteristic order of muscle involvement can be remembered by the mnemonic I'M SLOW
- bilateral (76-90%) and symmetric (70%) involvement is typical
- the anterior tendon is typically spared (although it can be involved in acute cases), with the swelling largely confined to the muscle belly
- this appearance is often referred to as 'coke bottle' in nature (Coca-Cola bottle sign), given its resemblance to the classic Coca-Cola bottle
- reference normal size range:
- inferior rectus: 3.2-6.5 mm
- medial rectus: 3.3-5.0 mm
- superior group: 3.2-6.1 mm
- lateral rectus: 1.7-4.8 mm
- the size of the muscles correlates with both the severity of disease and the risk of optic nerve compression
- increase in retro-ocular orbital fat
The greater the extraocular muscle bulk (especially medial rectus bulk nearer to the apex) and the longer and narrower the bony orbit, the more crowded the orbital apex will become. Apical crowding could result in optic nerve dysfunction/optic neuropathy due to optic nerve compression .
Other rarer signs include :
- enlargement of the lacrimal glands (lymphocytic infiltration)
- chemosis
- anterior displacement of the orbital septum
MRI
Evaluation with MRI may be useful due to improved soft-tissue contrast and multiplanar capabilities. MRI avoids ionizing radiation to the lens and corresponding increased risk of radiation-induced cataracts. Location and involvement of the ocular muscles generally follow the described CT appearances. Specific MRI sequences findings may include:
- T1: isointense to the other facial muscles, or fatty infiltration
- T2: increased signal intensity may be seen due to the inflammatory process
- T1 C+ (Gd): enhancement may be present
Treatment and prognosis
Although in many instances the disease is self-limiting, spontaneously improving within 2-5 years , discomfort, cosmetic issues, the risk of corneal ulceration, and optic nerve compression often require treatment. Options include:
- medical:
- supportive, steroids
- radiotherapy
- surgical decompression
Differential diagnosis
General imaging differential considerations include:
- orbital pseudotumor: involves the tendinous insertion
- orbital arteriovenous malformation
- orbital sarcoidosis
- orbital lymphoma
- orbital metastases
- orbital amyloidosis (rare)
- Erdheim Chester disease
Siehe auch:
- Morbus Basedow
- inflammatorischer Pseudotumor der Orbita
- orbitales Lymphom
- Nervus opticus
- Exophthalmus
- Erdheim-Chester-Erkrankung
- Metastasen in der Orbita
- Hashimoto-Thyreoiditis
- äußere Augenmuskulatur
- I'M SLOW
- coca-cola-bottle-sign
und weiter:

 Assoziationen und Differentialdiagnosen zu Graves ophthalmopathy:
Assoziationen und Differentialdiagnosen zu Graves ophthalmopathy: