Transitional cell carcinoma (urinary tract)










Transitional cell carcinoma (TCC), also called urothelial cell carcinoma (UCC), is the most common primary malignancy of the urinary tract and may be found along its entire length, from the renal pelvis to the bladder.
As imaging findings and treatment vary according to where along the urinary tract the tumor arises, each location is discussed separately.
- transitional cell carcinoma of the renal pelvis
- transitional cell carcinoma of the ureter
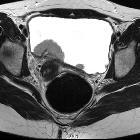
- transitional cell carcinoma of the bladder
- transitional cell carcinoma of the urethra
The remainder of this article concerns itself with a general discussion of transitional cell carcinomas.
Terminology
Some prefer the more general term "urothelial cell" carcinoma (UCC) to describe malignant bladder carcinomas of epithelial origin since 25-37% of "transitional cell" carcinomas contains a mixture of histologic tissue types .
Epidemiology
Transitional cell carcinoma is typically a tumor of older patients, with the average age of presentation being 65, and the majority of patients being over the age of 60 . There is a strong male predilection (M:F = 4:1), at least in part due to many tumors (especially historically) having been due to industrial exposure (see below).
A number of chemical compounds have been implicated in the development of uroepithelial tumors, including :
- smoking
- azo dye/pigment manufacturing
- beta-naphthylamine
- 4-aminobiphenyl
- 4-nitrobiphenyl
- 4,4-diaminobiphenyl
- cyclophosphamide (also causes hemorrhagic cystitis, and bladder fibrosis)
- Thorotrast
- phenacetin
- aristolochic acid (Balkan nephropathy): typically result in upper urinary tract tumors
- heavy caffeine consumption and artificial sweeteners were suggested as risk factors but most likely are not
Additionally, and acting synergistically with the above-mentioned factors is stasis, which presumably acts to prolong exposure of the urothelium to any carcinogens present in the urine. This also contributes to the higher frequency of transitional cell carcinomas in the bladder compared to the upper tracts.
- horseshoe kidney
- calculi: also associated with squamous cell carcinoma
- ureteral pseudodiverticulosis
- ureteritis cystica
Clinical presentation
Clinical presentation is variable and usually non-specific.
- hematuria: most common presenting symptom for upper tract tumors
- symptomatic hydronephrosis
- palpable pelvic mass
- strangury
- occasionally patients only present once systemic symptoms of metastatic disease are present
Distribution
The relative frequency of transitional cell carcinomas along the renal tract varies greatly, largely as a function of the surface area of each section :
- renal pelvis: uncommon ~2-3%
- ureter: least common ~1%
- bladder: by far the most common ~97%
Pathology
Transitional cell carcinomas of the have one of two main morphologic patterns:
- broad base with many frond-like papillary projections
- tend to be low grade and invasion beyond the mucosa is a late feature
- sessile or nodular tumors
- tend to be high grade with early invasion beyond the mucosa
Tumors are divided into three histological grades (see grading of TCCs). However, note should be made that stage is far more prognostically important than tumor grade .
Variants
Radiographic features
The radiographic features depend on the location of the tumor, and as such are discussed individually:
- transitional cell carcinoma of the renal pelvis
- transitional cell carcinoma of the ureter
- transitional cell carcinoma of the bladder
Treatment and prognosis
Treatment options vary with the location of the tumor, but in general, require surgical excision. Installation of bacille Calmette-Guerin (BCG) or mitomycin C may be used in selected cases as an alternative to surgery in some cases .
A critical part of the management of patients with transitional cell carcinomas is an awareness of the high rate of recurrence due to a field effect on the urothelium. Approximately 40% of patients with an upper urinary tract transitional cell carcinoma will go on to develop one or more TCCs of the bladder, and approximately 2-4% of patients with a bladder transitional cell carcinoma will go on to develop one or more TCCs of the renal pelvis or ureter .
Siehe auch:
- Hufeisenniere
- Transitionalzellkarzinom des Nierenbeckens
- balkan nephropathy
- transitional cell carcinoma of the ureter
- Transitionalzellkarzinom der Urethra
- Transitionalzellkarzinom der Blase
- staging of transitional cell carcinomas
- grading of TCCs
- calculi
und weiter:
- osteoblastische Knochenmetastasen
- genitourinary curriculum
- Superscan Szintigraphie
- Lymphom der Niere
- ureteritis cystica
- Harnblasenkarzinom
- medulläres Nierenkarzinom
- split bolus technique
- bladder calcification (mnemonic)
- TCC of the ureter
- Ursachen Nierenblutung
- Leiomyom der Harnblase
- transitional cell carcinoma grading
- Tumoren des Ureters
- Plattenepithelkarzinom der Harnblase
- aristolochic acid nephropathy
- Hämaturie
- stipple sign
- SCC of the bladder
- multiple Füllungsdefekte im Ureter
- Adenokarzinom der Harnblase

 Assoziationen und Differentialdiagnosen zu Urothelkarzinom:
Assoziationen und Differentialdiagnosen zu Urothelkarzinom:


