Hypertensive encephalopathy
 nicht verwechseln mit: reversibles zerebrales Vasokonstriktionssyndrom
nicht verwechseln mit: reversibles zerebrales Vasokonstriktionssyndrom ähnliche Suchen
ähnliche SuchenHypertensive encephalopathy
posterior reversible encephalopathy syndrome
reversible posteriore Leukoenzephalopathie
reversible posterior leukoencephalopathy
reversible posterior leukoencephalopathy syndrome (RPLS)
PRES
posterior reversible encephalopathy syndrome (PRES)
RPLS
reversible posterior leukoencephalopathy syndrome
Reversible posterior cerebral edema syndrome
Hyperperfusion encephalopathy
Occipito-parietal encephalopathy
Reversible leukoencephalopathy
Acute hypertensive encephalopathy
Reversible posterior cerebral oedema syndrome
 siehe auch
siehe auchsystemischer Lupus Erythematodes
Progressive multifokale Leukenzephalopathie
SMART syndrome
reversibles zerebrales Vasokonstriktionssyndrom
Mitochondriale Encephalomyopathie mit Lactatacidose und Schlaganfall-ähnlichen Episoden (MELAS)
Bluthirnschranke
sagittal sinus thrombosis
posteriore Leukoenzephalopathie
Hämolytisch-urämisches Syndrom
thrombocytopaenic thromboic purpura (TTP)
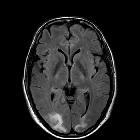
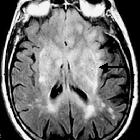
Posterior reversible encephalopathy syndrome (PRES), also known as acute hypertensive encephalopathy or reversible posterior leukoencephalopathy, is a neurotoxic statethat occurs secondary to the inability of the posterior circulation to autoregulate in response to acute changes in blood pressure. Hyperperfusion with resultant disruption of the blood brain barrier results in vasogenic edema, usually without infarction, most commonly in the parieto-occipital regions.
Terminology
The term posterior reversible encephalopathy syndrome may be a misnomer as the syndrome can involve or extend beyond the posterior cerebrum. Furthermore, although most cases involve a resolution of changes with the treatment of the precipitating cause and clinical recovery some patients can progress to develop permanent cerebral injury and be left with residual neurological defects.
It should not be confused with chronic hypertensive encephalopathy, also known as hypertensive microangiopathy, which results in microhemorrhages in the basal ganglia, pons, and cerebellum.
Clinical presentation
Patients may present with:
- headache
- seizures
- encephalopathy
- and/or visual disturbance
Pathology
Various clinical settings can precipitate the syndrome. The mechanism is not well understood but is thought to be related to the altered integrity of the blood brain barrier. Two main theories have been proposed:
- high blood pressure: leads to loss of self-regulation, hyperperfusion with endothelial damage and vasogenic edema
endothelial dysfunction: leads to vasoconstriction and hypoperfusion resulting in cerebral ischemia and subsequent vasogenic edema
Hypertension is not present or does not reach the upper limits to self-regulation (150-160 mmHg) in 25% of patients.
Etiology
- severe hypertension
- postpartum
- eclampsia/pre-eclampsia
- acute glomerulonephritis
- hemolytic-uremic syndrome (HUS)
- thrombocytopenic thrombotic purpura (TTP)
- systemic lupus erythematosus (SLE)
- drug toxicity
- cisplatin
- cyclophosphamide
- interferon
- erythropoietin
- tacrolimus
- cyclosporine
- azathioprine
- L-asparaginase
- filgrastim
- bone marrow or stem cell transplantation
- solid organ transplantation
- sepsis
- hyperammonemia
- sickle cell disease
- ventriculoperitoneal shunt insertion/overshunting
Microscopic appearance
- during the acute course of PRES: vasogenic edema, without inflammation, ischemia, or neuronal damage
during the late course of PRES: demyelination and myelin pallor along with evidence of ischemia, anoxic neuronal damage, laminar necrosis, or older hemorrhage in the white matter and cortex
Radiographic features
Most commonly there is vasogenic edema within the occipital and parietal regions (~95% of cases), perhaps relating to the posterior cerebral artery supply. The edema is usually symmetrical. Despite being termed posterior, posterior reversible encephalopathy syndrome can be found in a non-posterior distribution, mainly in watershed areas, including within the frontal, inferior temporal, cerebellar, and brainstem regions . Both cortical and subcortical locations are affected.
There are three main imaging patterns:
Other uncommon patterns of posterior reversible encephalopathy syndrome in <5% include: purely unilateral, or "central" (brainstem or basal ganglia lacking cortical or subcortical white matter involvement).
Parenchymal infarctions and hemorrhage are associated with posterior reversible encephalopathy syndrome in respectively 10-25% and 15% of cases.
The presence of contrast enhancement, no matter the pattern or how avid, does not portend the clinical outcome.
CT
The affected regions, as outlined above, are hypoattenuating.
Angiography (DSA)
There are signs of vasospasm or arteritis :
- diffuse vasoconstriction
- focal vasoconstriction
- vasodilatation
- string-of-beads appearance
MRI
Signal characteristics of affected areas usually reflect vasogenic edema, with some exceptions:
- T1: hypointense in affected regions
- T1 C+ (Gd): patchy variable enhancement. It can be seen in ~35% of patients, whether leptomeningeal or cortical pattern.
- T2: hyperintense in affected regions
- DWI: usually normal, sometimes hyperintense due to edema (T2 shine-through) or true restricted diffusion
- ADC: usually increased signal due to increased diffusion, but restricted diffusion is present in a quarter of cases
- GRE/SWI: may show hemorrhages in 9-50%
MRA may show patterns of vasculopathy with vessel irregularity consistent with focal vasoconstrictions/vasodilatation and diffuse vasoconstriction . MRV tend to be normal in posterior reversible encephalopathy syndrome .
History and etymology
Posterior reversible encephalopathy syndrome was described for the first time as a distinct entity in 1996 by an American neurologist Judy Hinchey et al . Although others had previously described similar reversible CT and MRI findings in hypertension back to the 1980s .
Differential diagnosis
General imaging differential considerations include:
- progressive multifocal leukoencephalopathy (PML)
- periventricular and subcortical involvement, sparing the cortex
- little or no mass effect or enhancement
- severe hypoglycemia
- posterior circulation infarct
- occipital and cerebellar involvement
- acute infarct demonstrates restricted diffusion; PRES typically does not restrict
- gliomatosis cerebri
- more asymmetric
- sagittal sinus thrombosis
- hypoxic-ischemic encephalopathy
- SMART syndrome
Siehe auch:
- Gliomatosis cerebri
- systemischer Lupus Erythematodes
- Progressive multifokale Leukenzephalopathie
- SMART syndrome
- reversibles zerebrales Vasokonstriktionssyndrom
- Mitochondriale Encephalomyopathie mit Lactatacidose und Schlaganfall-ähnlichen Episoden (MELAS)
- Bluthirnschranke
- sagittal sinus thrombosis
- posteriore Leukoenzephalopathie
- Hämolytisch-urämisches Syndrom
- thrombocytopaenic thromboic purpura (TTP)
und weiter:
 Assoziationen und Differentialdiagnosen zu posteriores reversibles Enzephalopathiesyndrom:
Assoziationen und Differentialdiagnosen zu posteriores reversibles Enzephalopathiesyndrom: