Caroli syndrome












Caroli disease and Caroli syndrome are congenital disorders comprising of multifocal cystic dilatation of segmental intrahepatic bile ducts. Caroli disease is limited to the dilatation of larger intrahepatic bile ducts, whereas Caroli syndrome describes the combination of small bile ducts dilatation and congenital hepatic fibrosis. However, some series show that extrahepatic duct involvement may exist. They are also classified as a type V choledochal cyst, according to the Todani classification.
Epidemiology
Caroli disease and Caroli syndrome are rare autosomal recessive disorders with a slight female predilection.
Clinical presentation
Presentation is in childhood or young adulthood. Caroli disease presents with right upper quadrant pain, recurrent cholelithiasis, and cholangitis with fever and jaundice. Caroli syndrome presents with the previous symptoms along with signs of portal hypertension, including hematemesis and melena secondary to bleeding varices.
Pathology
Pathologically, Caroli disease and Caroli syndrome belong to the spectrum of fibropolycystic liver disease which results from in utero malformation of the ductal plate . There is a high association with fibrocystic anomalies of the kidneys which share the same genetic defect (PKHD1 gene, chromosome region 6p21) .
The ductal plate is a layer of hepatic precursor cells that surround the portal venous branches and is the anlage of the intrahepatic bile ducts. The manifestation of ductal plate malformation depends on the level of the biliary tree that is affected .
Thus, Caroli disease (the simple type) results from the abnormal development of the large bile ducts.
In contrast, in Caroli syndrome (the periportal type of Caroli disease), both the central intrahepatic bile ducts and the ductal plates of the smaller peripheral bile ducts are affected, with the latter leading to the development of fibrosis.
At the other end of the fibropolycystic disease spectrum are von Meyenburg complexes, also known as biliary hamartomas which result from discrete foci of ductal plate malformation affecting the smallest bile ducts .
Associations
- simple Caroli disease is uncommon; it occurs more frequently with congenital hepatic fibrosis, constituting the Caroli syndrome
- medullary sponge kidney
- autosomal dominant polycystic kidney disease (ADPKD)
- autosomal recessive polycystic kidney disease (ARPKD)
Radiographic features
The disease may be diffuse, lobar or segmental. Dilatation is most frequently saccular rather than fusiform, a feature that might help in the differential diagnosis.
Ultrasound
- may show dilated intrahepatic bile ducts (IHBD)
- intraductal bridging: echogenic septa traversing the dilated bile duct lumen
- small portal venous branches partially or completely surrounded by dilated bile ducts
- the intraluminal portal vein sign: dilated ducts surrounding the portal vein
- intraductal calculi
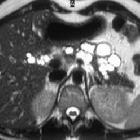
CT
- multiple hypodense rounded areas which are inseparable from the dilated intrahepatic bile ducts
- “central dot” sign: enhancing dots within the dilated intrahepatic bile ducts, representing portal radicles
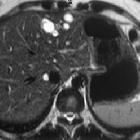
MRI
- T1: hypointense dilatation of IHBD
- T2: hyperintense
- T1 C+ (Gd): enhancement of the central portal radicles within the dilated IHBD
- MRCP: demonstrates continuity with the biliary tree
Nuclear medicine
Intrahepatic bile ducts can have a beaded appearance on HIDA scans .
Treatment and prognosis
Prognosis is generally poor. If the disease is localized, segmentectomy or lobectomy may be offered. In diffuse disease management if generally with conservative measures; liver transplantation may be an option .
Complications
- simple type
- intrahepatic stone formation
- recurrent cholangitis that may lead to bacteremia and sepsis
- hepatic abscesses
- periportal fibrosis type
- cirrhosis and portal hypertension
- hepatomegaly
- ascites
- varices
- there is an increased risk of cholangiocarcinoma, which develops in 7% of patients
History and etymology
It is named after Jacques Caroli (1902-1979), a French gastroenterologist, who described it in 1958 .
Differential diagnosis
- polycystic liver disease
- no associated biliary duct dilatation
- rarely communicate with the biliary ducts
- peribiliary cysts
- choledochal cyst
- biliary hamartomas
- may be cystic
- primary sclerosing cholangitis
- dilatation typically more fusiform and isolated;
- associated inflammatory bowel disease in 70% of caucasian patients
- recurrent pyogenic cholangitis
- both present with sepsis and biliary dilatation
- saccular (vs fusiform) dilatation favors Caroli disease
- obstructive biliary dilatation
For a further CT differential, consider also focal hypodense hepatic lesions on a non-contrast CT scan.
Siehe auch:
- Choledochuszyste
- Von-Meyenburg-Komplex
- Chronisch-entzündliche Darmerkrankungen
- Primär sklerosierende Cholangitis
- congenital hepatic fibrosis
- rezidivierende pyogene Cholangitis
- Zystenleber
- focal hypodense hepatic lesions on a non contrast CT scan
und weiter:
- Todani-Klassifikation der Gallengangszysten
- Differenzialdiagnosen zystischer Leberläsionen
- focal hypodense hepatic lesions on non-enhanced CT
- Gallengangatresie
- caroli disease and autosomal recessive polycystic kidney disease
- caroli disease with medullary sponge kidney and nephrocalcinosis
- Caroli's disease associated with medullary sponge kidney
- sekundäres oder postoperatives Caroli-Syndrom

 Assoziationen und Differentialdiagnosen zu Caroli-Syndrom:
Assoziationen und Differentialdiagnosen zu Caroli-Syndrom: