Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL)









Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL) is an autosomal dominant microvasculopathy characterized by recurrent lacunar and subcortical white matter ischemic strokes and vascular dementia in young and middle age patients without known vascular risk factors. There is disproportionate cortical hypometabolism.
Epidemiology
CADASIL is an autosomal dominant trait, with patients typically becoming symptomatic in adulthood (30 to 50 years of age).
Clinical presentation
Presentation is usually with recurrent transient ischemic attacks (TIAs) or strokes in multiple vascular territories. Presenile dementia and migraines develop in the third-to-fourth decades of life. Clinically, CADASIL often has a similar presentation to migraines and may also have auras. Depression, psychosis, pseudobulbar palsy and focal neurological defects as well as seizures are also seen .
Pathology
CADASIL results from a mutation on chromosome 19p13.12 involving the NOTCH3 gene, and as the name implies is inherited as an autosomal dominant trait. It results in small vessel and arteriole stenosis secondary to fibrotic thickening of the basement membrane of the vessels; the pathological hallmark is the deposition of granular osmiophilic material in close relation to the vascular smooth muscle cells .
Histology
An angiopathy of small and middle sized arteries is characteristic, without atherosclerosis or amyloid deposition . Diagnosis requires genetic identification of the mutated gene .
Radiographic features
CT
CT is non-specific, demonstrating white matter regions of low attenuation.
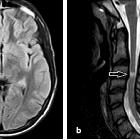
MRI
MRI is the investigation of choice, often demonstrating widespread confluent white matter hyperintensities . More circumscribed hyperintense lesions are also seen in the basal ganglia, thalamus and pons .
Although the subcortical white matter can be diffusely involved, in the initial course of the disease involvement of the anterior temporal lobe (86%) and external capsule (93%) are classical . There is relative sparing of the occipital and orbitofrontal subcortical white matter , subcortical U-fibers and cortex .
Cerebral microhemorrhages have been reported to occur in ~45% (range 25-70%) of cases without a characteristic distribution .
Eventually cerebral atrophy ensues, which correlates well with the degree of cognitive decline.
Treatment and prognosis
Typically the disease has a variable but progressive course leading to death between 50 to 70 years of age .
Differential diagnosis
General imaging differential considerations include:
- multiple early age infarcts from a hypercoagulable state
- MELAS
- subcortical arteriosclerotic encephalopathy (SAE)
- Susac syndrome
- CNS vasculitis
- COL4A1 brain small-vessel disease
- myotonic dystrophy type 1
Practical points
- think of it in younger patients with small vessel ischemic white matter change
- predilection for anterior temporal lobe white matter is a distinctive feature
- sparing of the cortex and subcortical U-fibers is typical
See also
Siehe auch:
- Zerebrale Amyloidangiopathie
- Encephalomyelitis disseminata
- Morbus Fabry
- subcortical arteriosclerotic encephalopathy (SAE)
- Susac syndrome
- Leukenzephalopathie
- Mitochondriale Encephalomyopathie mit Lactatacidose und Schlaganfall-ähnlichen Episoden (MELAS)
- Vaskulitis des Zentralen Nervensystems
und weiter:

 Assoziationen und Differentialdiagnosen zu CADASIL:
Assoziationen und Differentialdiagnosen zu CADASIL: