Rachitis


























Rickets, less commonly known as rachitis, refers to deficient mineralization of the growth plate in the pediatric population. In contrast, osteomalacia refers to deficient mineralization of the bone matrix, which co-occurs with rickets but can also occur even after growth plate closure, in adults .
Epidemiology
Rickets is seen in a number of distinct populations :
- premature infants (especially if on parenteral nutrition)
- unbalanced infant nutrition
- protracted exclusive breastfeeding
- non-vitamin D supplemented formula-fed infants
- vegetarian diets
- maternal vitamin D deficiency
- lack of sun exposure
- dark skin in sun-poor countries
- lack of outdoor time
- clothing that eliminates sun exposure
The onset and presentation of rickets depend on the etiology and degree of deficiency. Typically, in severe cases, rickets becomes apparent in the second year of life.
Clinical presentation
The presentation is usually with skeletal changes (see below) and bone pain.
Pathology
Abnormalities in calcium-phosphate homeostasis disrupt endochondral ossification at open physes. The etiologies can be classified by whether the initial abnormality is inadequate calcium absorption or excessive phosphate excretion, termed "calcipenic" and "phosphopenic" rickets, respectively . The serum laboratory abnormalities are characteristic:
- calcipenic rickets
- parathyroid hormone: markedly elevated
- calcium: low or normal
- phosphate: low or normal
- phosphopenic rickets
- parathyroid hormone: normal or modestly elevated
- calcium: normal
- phosphate: low
Calcipenic rickets etiologies are the most common:
- vitamin D deficiency (most common cause) due to diet, insufficient sun exposure, and/or malabsorption
- dietary calcium deficiency
- defective vitamin D metabolism: mutation in CYP27B1 gene, which encodes the renal 1-alpha-hydroxylase enzyme (vitamin D dependent rickets type 1); 25-hydroxylase deficiency (very rare)
- hereditary vitamin D resistance: mutation in VDR gene, which encodes the vitamin D receptor (vitamin D dependent rickets type 2)
Phosphopenic rickets etiologies are usually associated with elevated circulating fibroblast growth factor 23 (FGF23) levels and/or renal tubule disorders:
- hereditary hypophosphatemic rickets (vitamin D resistant rickets)
- tumor-induced (oncogenic) rickets
- Fanconi syndrome
Radiographic features
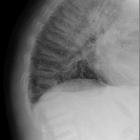
In the growing skeleton, the deficiency of normal mineralization is most evident at metaphyseal zones of provisional calcification where there is an excess of non-mineralized osteoid resulting in growth plate widening and abnormal configuration of the metaphysis:
- fraying: indistinct margins of the metaphysis
- splaying: widening of metaphyseal ends
- cupping: concavity of metaphysis
It is not surprising that these features are most prominent at the bones where growth is greatest:
- knee: distal femur, proximal tibia
- wrist: especially the ulna
- anterior rib ends: rachitic rosary
As osteomalacia co-occurs with rickets, it is important to remember that even bones that appear mineralized are weak and result in bowing, most commonly seen in the lower limbs once the child is walking. The legs bow outwards with variable deformity of the hips (both coxa vara and coxa valga are seen ). Other bone deformities are also noted such as genu valga and vara as well as protrusio acetabuli . The lower ribs may also be drawn inwards inferiorly by the attachment of the diaphragm (Harrison's sulcus).
A mnemonic to help remember these features is RICKETS.
Treatment and prognosis
Treatment requires correction of the metabolic imbalance. Only rarely is the orthopedic surgical intervention necessary to correct skeletal deformities.
Post-treatment
Radiographic features of rickets lag behind biochemical and clinical improvements by about 2 weeks. Harris growth arrest line is a dense line traversing parallel to the metaphysis which can be used as a marker of old rickets .
Differential diagnosis
The differential for leg bowing in children includes :
- developmental or congenital bowing
- Blount disease
- osteogenesis imperfecta
- many others that are not usually a consideration (see leg bowing in children)
The differential for a widening of the growth plate includes:
- Schmid-type metaphyseal chondrodysplasia
- hypovitaminosis C (scurvy)
- delayed maturation due to illness
- endocrine disturbances
- growth hormone excess
- hyperparathyroidism
- hypothyroidism
The differential for flaring of the metaphysis includes:
- anemias
- fibrous dysplasia
- storage diseases
- chronic lead poisoning
- bone dysplasias
Siehe auch:
- Osteogenesis imperfecta
- rachitischer Rosenkranz
- primärer Hyperparathyreoidismus
- Biegungsbruch
- Osteomalazie
- Morbus Blount
- dichte metaphysäre Bänder
- Vitamin D
- Tibiaverbiegung bei Kindern
- Skorbut
- Verbiegung der langen Röhrenknochen
- Bleivergiftung
- Rickets (mnemonic)
- Knochendysplasie
- Vitamin-D-Mangel
- aufgetriebene Metaphysen
und weiter:
- Basiläre Impression
- Protrusio acetabuli
- Wormsche Knochen
- Loosersche Umbauzonen
- Auftreibung Metaphysen
- Sprengel-Deformität
- alternating radiolucent and radiodense metaphyseal lines
- Hypophosphatasie
- Platybasie
- premature closure of a growth plate
- basilar invagination (mnemonic)
- verzögerte Skelettreifung
- osteoid
- Erlenmeyer flask deformity of the femur
- Vitamin-D resistente Rachitis
- wormian bones (mnemonic)
- transverse metaphyseal lines (mnemonic)
- De-Toni-Fanconi-Syndrom
- Metaphysäre Chondrodysplasie Typ Jansen
- Metaphysäre Chondrodysplasie
- differential diagnosis of generalized osteopaenia
- generalised osteopaenia
- Harrison-Sulcus
- Auftreibung der Rippen

 Assoziationen und Differentialdiagnosen zu Rachitis:
Assoziationen und Differentialdiagnosen zu Rachitis: