transient splenial lesion of corpus callosum associated with discontinuation of antiepileptic therapy
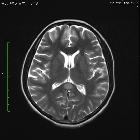


transient splenial lesion of corpus callosum associated with discontinuation of antiepileptic therapy
Cytotoxic lesions of the corpus callosum (CLOCCs) Radiopaedia • CC-by-nc-sa 3.0 • de
Cytotoxic lesions of the corpus callosum (CLOCCs) represent a collection of disparate conditions that can cause signal change in the corpus callosum, usually involving the splenium.
Terminology
The term cytotoxic lesions of the corpus callosum (CLOCCs) has been proposed recently as a more precise description of this phenomenon which has previously been known by a variety of terms including transient lesions of the splenium of the corpus callosum, mild encephalitis/encephalopathy with a reversible isolated SCC lesion (MERS), reversible splenial lesions and reversible splenial lesion syndrome (RESLES). CLOCCs not only better reflects current understanding of the underlying pathophysiology of these lesions but also does not explicitly imply that these lesions are confined to the splenium. As such it is probably a better term to use.
Clinical presentation
Clinical presentation relates to the underlying pathology (see below) rather than to the callosal lesion itself. Unlike many other lesions of the corpus callosum, CLOCCs do not demonstrate convincing signs or symptoms of hemispheric disconnection, such as pseudo-neglect, alien hand syndrome, apraxia of the left hand, agraphia, alexia, and visual apraxias .
Pathology
Although numerous underlying etiologies have been identified, these lesions appear to result from a stereotyped cascade of cytokines and stimulated cells. An initial insult results in macrophages releasing inflammatory cytokines (IL-1 and IL-6) which in turn result in a cascade of changes including recruitment T-cells, break-down of the blood-brain barrier, production of TNF-α, and activation of astrocytes. The end result is a massive increase in glutamate in the extracellular fluid which, via interactions with a number of cell membrane receptors, results in an influx of water into both astrocytes and neurons which manifests macroscopically as cytotoxic edema .
It appears that the reason the splenium of the corpus callosum is preferentially affected is the presence of a high density of oligodendrocytes expressing large numbers of glutamate affected receptors .
Etiology
Cytotoxic lesions of the corpus callosum are seen in a wide variety of clinical settings, although exactly which conditions are listed in any one publication varies. Classically CLOCCs are seen in patients with seizures or metabolic disturbances, although many other etiologies are recognized. Reported etiologies include :
- seizures
- complex relationship – CLOCCs seen in a variety of settings:
- antiepileptic medications (with or without seizures)
- sudden cessation of antiepileptic drugs (classic)
- seizures with or without antiepileptic medications
- complex relationship – CLOCCs seen in a variety of settings:
- metabolic disturbance
- electrolyte imbalance (e.g. hyperammonemia, hyper- and hyponatremia)
- hemolytic-uremic syndrome
- hepatic encephalopathy
- hypoglycemia
- Marchiafava-Bignami disease
- osmotic demyelination (e.g. extrapontine myelinolysis )
- Wernecke encephalopathy
- Wilson disease
- infections
- reported in a wide range of cerebral infections, including cerebral abscess, encephalitis and meningitis
- viral (e.g. influenza, measles, herpes, mumps, adenovirus, varicella zoster, rotavirus, SARS-CoV-2)
- bacterial (e.g. salmonella, Legionnaires' disease)
- mycobacterial (e.g. tuberculous meningitis)
- reported in a wide range of cerebral infections, including cerebral abscess, encephalitis and meningitis
- CNS malignancy
- many are associated with chemotherapy and/or seizures
- drugs and toxins
- antidepressants (e.g amitriptyline)
- antiepileptics (e.g. carbamazepine, lamotrigine, phenytoin)
- antipsychotics (e.g. clozapine)
- chemotherapy (e.g. cyclosporin, fluorouracil)
- corticosteroids
- pesticide (e.g. methyl bromide)
- subarachnoid hemorrhage
- especially if large volume
- not the result of vasospasm
Radiographic features
Transient lesions of the splenium are only really appreciable on MRI where they have three distinct patterns :
The smaller well-circumscribed lesions are the typical lesion seen in the setting of seizures/cessation of antiepileptic medication, whereas the larger lesion is more typical of other etiologies.
MRI
These lesions demonstrate the expected features of cytotoxic edema :
- T1: hypointense
- T2: hyperintense
- DWI/ADC: restricted diffusion (ADC typically 300–500 x 10 mm/s)
- T1 C+ (Gd): no enhancement
Some studies have shown that patients generally recover completely on MRI studies within 1 month, mostly within 1 week following the neurological recovery .
Treatment and prognosis
The prognosis generally depends on the underlying cause, but in the setting of epilepsy or antiepileptic drug-related lesions, it is very good.
Differential diagnosis
Depending on the publication, some of the differentials to contemplate are included in the list of etiologies of CLOCCs. In any case, when confronted with a splenial lesion consider:
- demyelination
- infarction (e.g. pericallosal artery occlusion)
- posterior reversible encephalopathy syndrome (PRES)
- trauma (e.g. diffuse axonal injury)
- tumors (e.g. diffuse glioma, lymphoma)
Siehe auch:

 Assoziationen und Differentialdiagnosen zu transient splenial lesion of corpus callosum associated with discontinuation of antiepileptic therapy:
Assoziationen und Differentialdiagnosen zu transient splenial lesion of corpus callosum associated with discontinuation of antiepileptic therapy:
