Acute Respiratory Distress Syndrome







































Acute respiratory distress syndrome (ARDS) is a form of acute lung injury and occurs as a result of a severe pulmonary injury that causes alveolar damage heterogeneously throughout the lung. It can either result from a direct pulmonary source or as a response to systemic injury.
Terminology
ARDS has a similar clinical presentation and histological features of those seen in acute interstitial pneumonitis (AIP), showing extensive diffuse alveolar damage (DAD). Both conditions likely represent the same pathology, with AIP probably accounting for some of the idiopathic cases of ARDS.
Pathology
Lung damage results in leakage of fluid into alveoli, leading to non-cardiogenic pulmonary edema and decreased arterial oxygenation.
The diagnosis is based on mainly clinical criteria set forth by the American-European Consensus Conference . Acute respiratory distress syndrome is characterized by the following criteria :
- lung injury of acute onset, within one week of an apparent clinical insult and with the progression of respiratory symptoms
- bilateral opacities on chest imaging not explained by other pulmonary pathology (e.g. pleural effusion, pneumothorax, or nodules)
- respiratory failure not explained by heart failure or volume overload
- decreased arterial PaO2/FiO2 ratio
- mild ARDS: 201-300 mmHg (≤39.9 kPa)
- moderate ARDS: 101-200 mmHg (≤26.6 kPa)
- severe ARDS: ≤100 mmHg (≤13.3 kPa)
It is of note that the clinical diagnosis of ARDS using internationally accepted guidelines and chest radiographs has been demonstrated to correlate poorly with histopathological diagnosis at autopsy .
Etiology
The causes of ARDS can result from a direct lung injury, termed pulmonary ARDS, or extrapulmonary where the triggering insult is outside of the lungs. These two etiological subtypes respond in different ways to mechanical ventilation. Some authors have described distinct early phase radiological appearances between the two.
Pulmonary causes
- fat embolism
- near-drowning
- viral pneumonia
- oxygen toxicity
- smoke inhalation
- disseminated intravascular coagulopathy
- aspiration of gastric contents
- aspiration of barium contrast
- lung contusion
Extrapulmonary causes
- pancreatitis
- burns
- trauma
- sepsis
- hypovolemic shock
- head injury
- transfusion reaction
- cardiopulmonary bypass
- abdominal compartment syndrome
Radiographic features
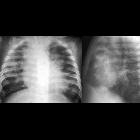
Plain radiograph
Chest radiographic findings of acute respiratory distress syndrome are non-specific and resemble those of typical pulmonary edema or pulmonary hemorrhage. There are diffuse bilateral coalescent opacities (the only radiological criterion defined by the Consensus Conference). The time course of ARDS may help in differentiating it from typical pulmonary edema.
Chest x-ray features usually develop 12-24 hours after initial lung insult as a result of proteinaceous interstitial edema. Within one week, alveolar pulmonary edema (hyaline membrane) occurs due to type 1 pneumocyte damage.
In contrast to cardiogenic pulmonary edema, which clears in response to diuretic therapy, ARDS persists for days to weeks. Also, as the initial radiographic findings of ARDS clear, the underlying lung appears to have a reticular pattern secondary to type 2 pneumocyte proliferation and fibrosis .
CT
Features depend on the phase of the disease .
Early phase
- pulmonary opacification: often demonstrates an anteroposterior density gradient within the lung, with dense consolidation in the most dependent regions, merging into a background of widespread ground-glass attenuation and then normal or hyperexpanded lung in the non-dependent regions (described as a classical appearance )
- the typical CT presentation of bilateral symmetrical changes is more common in extrapulmonary ARDS, whereas in pulmonary ARDS the opacities tend to be asymmetrical
- ground-glass opacification: a non-specific sign that reflects an overall reduction in the air content of the affected lung. In acute ARDS likely represent edema and protein within the interstitial and alveolar spaces
- bronchial dilatation within areas of ground-glass opacification
- some publications also report pulmonary cysts in the early phase
Postulated reason for inhomogeneity of appearances:
- increased weight of overlying lung causing compressive atelectasis posteriorly, which produces dense opacification
- supported by the fact that with the positional change from supine to prone, the density gradient can quickly redistribute accordingly
In the non-dependent portions, the lung may be of normal attenuation, or it may be lower if being mechanically ventilated.
Late phase and appearances in long-term survivors
CT appearances can be variable in this phase:
- complete resolution: may occur in some cases
- coarse reticular pattern and ground-glass opacification in the anterior (non-dependent) part of the lungs: considered more typical later stage CT appearances
- areas of reticular and ground-glass opacification
- pulmonary cysts of varying sizes and bullae (probably develop as a result of prolonged ventilation)
Classification
One described method is the Ichikado CT scoring of acute respiratory distress syndrome.
Treatment and prognosis
Acute respiratory distress syndrome carries high mortality of around 50% and many survivors develop chronic lung disease, with the damaged lung healing by fibrosis. However, a minority does make a full recovery.
History and etymology
It was first described in 1967 by Dave G Ashbough (fl. 2019) et al .
Siehe auch:
- Bronchopneumogramm
- Lungenödem
- Pankreatitis
- Persistierender Ductus arteriosus
- Herzfehler
- Lungenblutung
- fetal conditions associated with maternal diabetes
- interstitielles Lungenemphysem
- TRALI
- Bronchopulmonale Dysplasie
und weiter:
- right middle lobe consolidation
- Lungenfibrose
- Milchglasverschattungen
- crazy paving-Muster
- komplette Verschattung Hemithorax
- Parenchymband
- neonatal chest radiograph in the exam setting
- medikamenteninduzierte Pneumonitis
- acute bilateral airspace opacification
- Akute interstitielle Pneumonie
- Schock (Medizin)
- pulmonale Kryptokokkose
- PIE
- nicht-kardiogenes Lungenödem
- pulmonary manifestations of antiphospholipid syndrome
- Acute Respiratory Distress Syndrome neonatal
- respiratory distress syndrome of the newborn

 Assoziationen und Differentialdiagnosen zu acute respiratory distress syndrome (ARDS):
Assoziationen und Differentialdiagnosen zu acute respiratory distress syndrome (ARDS):