Budd-Chiari-Syndrom
























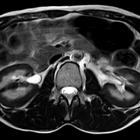
Budd-Chiari syndrome, also known as hepatic venous outflow obstruction (HVOO), refers to the clinical picture that occurs when there is partial or complete obstruction of the hepatic veins. It is characterized on imaging by ascites, caudate hypertrophy, peripheral atrophy, and prominent collateral veins.
Epidemiology
Budd-Chiari syndrome is rare. A Japanese study estimated the prevalence to be in the region of 2.4 cases/million . In Western populations, the most common cause is thrombosis. Membranous webs have been increasingly described in Asian patients as a cause of obstruction.
Clinical presentation
The classic acute presentation is with the clinical triad of ascites, hepatomegaly, and abdominal pain, although this is non-specific. The presentation may be acute or chronic:
- acute: results from an acute thrombosis of the main hepatic veins or the inferior vena cava; patients may present with rapid onset ascites
- chronic: the chronic form is related to fibrosis of the intrahepatic veins, presumably related to inflammation
Pathology
Etiology
The etiology is mixed and varied. The majority of cases result from thrombosis within the hepatic veins. However, 25% arise from external compression that results in obstruction:
- idiopathic (one-third of cases)
- congenital
- hepatic vein or inferior vena cava webbing
- interruption of the diaphragm
- venous thrombosis secondary to
- dehydration
- sepsis
- polycythemia rubra vera
- antiphospholipid syndrome
- pregnancy and the postpartum state
- oral contraceptive pill use
- sickle cell disease
- thrombocytosis
- paroxysmal nocturnal hemoglobinuria (PNH)
- injury and/or inflammation secondary to
- phlebitis: bone marrow transplant and chemoradiotherapy
- autoimmune disease
- tumor invasion, e.g. renal cell carcinoma, hepatocellular carcinoma, adrenal carcinoma
- leiomyosarcoma of inferior vena cava
It may be associated with concurrent portal vein thrombosis.
Radiographic features
Ultrasound
- acute
- hepatomegaly
- splenomegaly
- heterogeneous echotexture
- chronic
- hypertrophied caudate lobe
- peripheral atrophy of affected regions
- regenerative nodules: mostly corresponding to focal nodular hyperplasia-like lesions and therefore sharing similar imaging characteristics of these lesions
- usually multiple and smaller than 3 cm
- gallbladder wall thickening
- ascites
Color Doppler
- no flow or inappropriately directed flow in the right hepatic vein or a part of it
- discontinuity between the main hepatic vein and the inferior vena cava
- reversed flow in hepatic veins
- intra- and extrahepatic collaterals
- portal vein changes e.g. hepatofugal flow
- low or absent flow in the inferior vena cava or balanced bidirectional flow
- bland thrombus or tumor thrombus within the inferior vena cava
- increased resistive index within the hepatic artery: >0.75
CT
- early enhancement of the caudate lobe and central liver around the inferior vena cava
- delayed enhancement of the peripheral liver with accompanying central low density (flip-flop appearance)
- inhomogeneous mottled liver (nutmeg liver)
- peripheral zones of the liver may appear hypoattenuating because of reversed portal venous blood flow
- inability to identify hepatic veins
- in the chronic phase, there is caudate lobe enlargement and atrophy of the peripheral liver in affected areas
Angiography (DSA)
On hepatic venography:
- complete occlusion of hepatic vein(s)
- may or may not be associated with a (focal) stenosis of the intrahepatic inferior vena cava
- spider web appearance of the intrahepatic collateral veins
Treatment and prognosis
If left untreated, progression to liver failure from fibrosis and eventual death may occur. Management options include:
- liver transplantation (definitive treatment)
- surgical portosystemic shunting
- long-term anticoagulation
- hepatic venoplasty with stenting
- IVC-plasty with stenting
- transjugular intrahepatic portosystemic shunts (TIPS)
- as a bridging therapy prior to liver transplantation or surgical portosystemic shunting
- as a treatment for patients with contraindications for liver transplantation
Complications
Patients with chronic Budd-Chiari syndrome are at risk for hepatocellular carcinoma (HCC) and therefore should be monitored with serum alpha-fetoprotein (AFP) .
History and etymology
Initially described by Budd in 1845 before Chiari lent his first pathological description of "obliterating endophlebitis of the hepatic veins" in 1899.
Siehe auch:
- Nierenzellkarzinom
- Hypertrophie des Lobus caudatus
- Splenomegalie
- hepatozelluläres Karzinom
- Pfortaderthrombose
- Sichelzellenanämie
- Zwerchfell
- Aszites
- Leiomyosarkom
- Nebennierenrindenkarzinom
- transjugulärer intrahepatischer portosystemischer Shunt
- Paroxysmale nächtliche Hämoglobinurie
- Muskatnussleber
- Membranstenose Vena cava inferior
und weiter:

 Assoziationen und Differentialdiagnosen zu Budd-Chiari-Syndrom:
Assoziationen und Differentialdiagnosen zu Budd-Chiari-Syndrom: