Lobärblutung







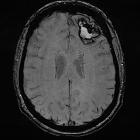


Lobar hemorrhage is a subtype of intracranial hemorrhage, which generally carries a poor prognosis.
Epidemiology
Primary lobar hemorrhages, usually due to cerebral amyloid angiopathy, are typically seen in elderly patients. Younger patients may also develop lobar hemorrhages, but in such cases there is usually an underlying lesion (e.g. cerebral arteriovenous malformation) .
Clinical presentation
Patients typically present with acute neurological deterioration, often with decreased GCS. Headache may be present.
Pathology
Etiology
Often the cause of a lobar hemorrhage is never established and the causes, when found, are varied including :
- cerebral amyloid angiopathy
- hypertension
- primary
- secondary to drug use (e.g. cocaine, amphetamines)
- cerebral aneurysm: both saccular and mycotic
- arteriovenous malformation
- cerebral cavernoma
- brain tumor
- bleeding disorders or coagulopathies
- anticoagulation - therapeutic or supratherapeutic levels
- vasculitis
- cerebral venous thrombosis
One of the strongest predictors of an underlying vascular lesion is the patient's age. The younger a patient, the more likely there is an identifiable cause: CTA found causes for hemorrhage in 47% of patients aged 18-45 years, 15% aged 46-70 years, and 4% aged 71-94 .
Radiographic features
Overall features of the hemorrhage that suggest an underlying secondary cause are :
- internal density heterogeneity
- highly irregular margin
- fluid-fluid level
- internal hematocrit level
- extensive surrounding vasogenic edema
- extensive subarachnoid hemorrhage
CT
CT is usually the modality first obtained and demonstrates a hyperdense collection of blood, located superficially within the lobes of the brain (i.e. not in the basal ganglia). The hemorrhages vary widely in size from only a centimeter or so (often asymptomatic) to extremely large hematomas, and can be estimated using ABC/2 and related formulas.
Extension into the subdural or subarachnoid and even intraventricular space may be seen. Intraventricular extension is far more common in basal ganglia hemorrhages.
CT angiography
It is becoming increasingly used in the workup of patients, not only to assess for an underlying abnormality but also to evaluate for the presence of a spot, the so-called CTA spot sign, that is indicative of ongoing bleeding. The presence of such a spot sign correlates, not surprisingly, with a growth of the hemorrhage in the first few hours following the scan and is, again not surprisingly, associated with a poor outcome .
CT perfusion
Recent studies have demonstrated the presence of the spot sign on dynamic-enhancement CT (DECT or CT perfusion) to be an even stronger predictor of hematoma expansion , i.e. the most robust factor in predicting outcome .
MRI
MRI is usually obtained when concern exists that the bleed is from an underlying lesion. Findings depend on the size and age of the bleed (see aging blood on MRI).
In cases of primary lobar hemorrhage, multiple small areas of susceptibility-induced signal drop-out may be evident on GRE or SWI, in-keeping with previous cerebral microhemorrhages, suggestive of cerebral amyloid angiopathy.
The presence of single lobar hemorrhage is still part of the Boston criteria for CAA.
Treatment and prognosis
Treatment depends on the age of the patient and the size and location of the hematoma. Medical management is the mainstay, often palliative if the bleed is enormous, or the patient has significant pre-existing co-morbidities.
Surgical evacuation may be necessary.
Differential diagnosis
The term lobar hemorrhage is often used to denote a primary hemorrhage. As such the differential includes:
- an underlying tumor (e.g. glioblastoma, cerebral metastasis)
- an underlying vascular malformation (e.g. cerebral arteriovenous malformation)
- hemorrhagic transformation of a cerebral infarct
- hemorrhagic transformation of the venous infarct
Video
Siehe auch:
- Hirnmetastase
- Intrazerebrale Blutung
- Glioblastoma multiforme
- Zerebrale Amyloidangiopathie
- zerebrale arteriovenöse Malformation
- Hirnblutung mit Ventrikeleinbruch
- venöser zerebraler Infarkt
- intrazerebrale Blutung bei Amyloidangiopathie
- zerebraler Mittellinienshift
und weiter:

 Assoziationen und Differentialdiagnosen zu Lobärblutung:
Assoziationen und Differentialdiagnosen zu Lobärblutung:






