neuroendokrine Pankreastumoren




























Endocrine tumors of the pancreas, also known as pancreatic neuroendocrine tumors (pNET), arise from the pancreatic islet cells and include some distinct tumors that match the cell type of origin.
Terminology
Pancreatic endocrine tumors have commonly been referred to as "islet cell tumors", referring to the islets of Langerhans, from which they were thought to derive. It has since been shown that these tumors derive from ductal pluripotent stem cells, and "endocrine tumor" is now preferred .
Epidemiology
Overall, pancreatic endocrine tumors have an incidence of 0.001% and account for 1-2% of pancreatic neoplasms. They occur most commonly at ages 30-60, with no clear gender predilection.
Associations
Most tumors are isolated. Approximately 1-2% are associated with the multiple endocrine neoplasia type I (MEN I), which is characterized by the triad of parathyroid, pituitary, and pancreatic lesions.
There are also associations between pancreatic endocrine tumors, von Hippel-Lindau disease and tuberous sclerosis.
Clinical presentation
Syndromic tumors tend to present earlier, with clinical signs and symptoms related to their cell type and biological activity:
- insulinoma: Whipple triad
- gastrinoma: Zollinger-Ellison syndrome
- glucagonoma: 4D syndrome
- non-functioning tumors: tend to present late and often larger in size
Pathology
Neuroendocrine tumors are classically defined by the expression of markers of neuroendocrine differentiation (including chromogranin A and synaptophysin) and hormone production.
These tumors can broadly be divided according to whether or not they secrete enough active compounds to be syndromic or not:
- syndromic tumors
- insulinoma: most common
- gastrinoma: second most common
- glucagonoma
- VIPoma: rare
- somatostatinoma: rare, some of these can be non-functional
- non-syndromic tumors: third most common
Individual functional tumors are discussed in more detail separately.
The term "syndromic" is preferred over "functioning" since it is becoming increasingly clear that most tumors are functional (i.e. produce hormones), but either do not produce enough hormone or produce an ineffective form of the hormone, so that they may not produce a clinical syndrome.
Classification
According to the 2017 World Health Organization (WHO) classification, these tumors are histologically graded as :
- well-differentiated status
- grade 1 (G1): tumor expressing < 2 mitoses/2mm and ≤ 2% Ki-67 index
- grade 2 (G2): tumor expressing between 2 to 20 mitoses/2mm and 3 to 20% Ki-67 index
- grade 3 (G3): more than 20 mitoses/2mm and more than 20% Ki-67 index
- poorly-differentiated and containing components of adenocarcinoma - they are named pancreatic neuroendocrine carcinoma (pNEC) and divided into two types
- small cell type
- large cell type
Radiographic features
Overall these endocrine tumors of the pancreas tend to be highly vascular and well-circumscribed, often displacing adjacent structures. They can demonstrate calcific or cystic change.
Ultrasound
- well-circumscribed with smooth margins
- round or oval
- hypoechoic
Liver metastases may be hyperechoic or targetoid.
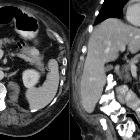
CT
Smaller tumors:
- hypervascular
- tend to be homogenous and well-circumscribed
Larger tumors:
- may appear heterogeneous and contain areas of cystic or necrotic change
- can occasionally manifest as primarily cystic lesions and are distinguishable from other cystic neoplasms by their hypervascular rim
Since usually have a distinct capsule which means they displace rather than invade surrounding structures as they grow in size. As a result, they less frequently present with biliary obstruction, which is a classic mode of presentation for pancreatic adenocarcinomas.
Endocrine tumors of the pancreas show peak contrast enhancement in the early arterial phase (25-35 s) rather than in late arterial phase (35-45 s) which is normally used for pancreatic imaging. This is particularly important when considering that small lesions may be missed in the late arterial phase when the tumor will appear isointense with enhancing pancreatic parenchyma.
MRI
Sensitivity is similar to CT
- T1: hypointense relative to pancreas
- T2: typically hyperintense relative to the pancreas, but there is a range of signal intensities
- T1 C+ (Gd): hyperintense/hypervascular relative to pancreas
- DWI/ADC: restricted diffusion is usually present and tends to correlate to the degree of tumor differentiation
Nuclear medicine
Nuclear medicine studies play an important role in the staging of neuroendocrine tumors.
- Gallium-68 DOTATATE (or DOTATOC, or DOTANOC) PET-CT
- superior to octreotide scan
- F-18 FDG PET-CT
- sensitivity limited unless poorly-differentiated
- Indium-111 octreotide
- planar or SPECT
- sensitivity is ~80%, although limited by the somatostatin receptor characteristics of the tumor
- reported sensitivity is highest with gastrinomas >2 cm
- reported sensitivity is lowest with insulinomas
- has been largely replaced by PET-CT in most centers
Treatment and prognosis
If diagnosed early enough (before metastases), then complete surgical resection may be curable. Even patients with advanced disease can have reasonable long-term survival. Biological behavior also depends on the cell of origin:
- insulinoma: 10% malignant
- gastrinoma: 60% malignant
- glucagonoma: 80% malignant
- VIPoma: 75% malignant
- somatostatinoma: 75% malignant
- non-functional: 85-100% malignant
Differential diagnosis
- metastasis (e.g. renal cell carcinoma)
- intrapancreatic splenule (if in the tail of the pancreas)
- mostly-solid serous cystadenoma
Practical points
check for concomitant metastatic disease: neuroendocrine tumors most commonly give metastases in the liver and, less frequently, in the bones
Siehe auch:
- Pankreaskarzinom
- Insulinom
- Pankreastumoren
- Gastrinom
- Hypervaskularisierte Pankreasläsionen
- multiple endokrine Neoplasie Typ 1
- Neuroendokriner Tumor
- solide Pankreastumoren
- Glukagonom
- Somatostatin-Rezeptor-Szintigrafie
- benigne Pankreastumoren
- Whipple-Trias
- Pankreasmetastasen (Nierenzellkarzinom)
- Somatostatinom
- VIPom
- zystischer neuroendokriner Tumor des Pankreas
und weiter:

 Assoziationen und Differentialdiagnosen zu neuroendokrine Pankreastumoren:
Assoziationen und Differentialdiagnosen zu neuroendokrine Pankreastumoren:









