Tuberculosis (intracranial manifestations)





















































Tuberculosis of the central nervous system can result from either haematogenous spread from distant systemic infection (e.g. pulmonary tuberculosis) or direct extension from local infection (e.g. tuberculous otomastoiditis).
Intracranial manifestations of tuberculosis are protean and can affect all compartments and are discussed individually in separate articles. Manifestations include:
- extra-axial
- tuberculous meningitis (leptomeningitis): most common
- tuberculous pachymeningitis: rare
- intra-axial
- intracranial tuberculous granuloma (tuberculoma)
- focal tuberculous cerebritis
- intracranial tuberculous abscess
- tuberculous rhombencephalitis
- tuberculous encephalopathy
The remainder of this article is a general discussion of CNS tuberculosis. For a general discussion on systemic tuberculosis, please refer to the article on tuberculosis.
Epidemiology
Tuberculosis remains a leading cause of morbidity and mortality in the developing world. It may account for ≈1/6 of the 3 million of global mortality due to Mycobacterium tuberculosis infection. CNS involvement is thought to occur in 2-5% of patients with tuberculosis and up to 15% of those with AIDS-related tuberculosis .
Although CNS involvement by tuberculosis is seen in all age groups, there is a predilection for younger patients, with 60-70% of cases occurring in patients younger than 20 years of age .
In endemic regions, tuberculomas account for as many as 50% of all intracranial masses .
Clinical presentation
Clinical presentation depends on the particular manifestation, although in all cases symptoms and signs are nonspecific and include fever, seizures, meningism and focal neurological deficits (e.g. altered sensorium, hemiparesis).
Pathology
Haematogenous spread from the lungs or gastrointestinal tract is most common, leading to small subpial or subependymal infective foci. These are termed Rich foci and form a reservoir from which intracranial manifestations may arise . This can occur either during the primary infection (uncommon, and more frequently seen in children) or be reactivated later and cause a post-primary infection.
Radiographic features
There is a wide radiological and pathological spectrum of the CNS disease. Tuberculous meningitis and intracranial tuberculous granuloma (tuberculoma) are the most common manifestations and these are discussed in detail in separate articles. Below is a brief discussion of the main imaging features of each presentation.
Tuberculous meningitis
Tuberculous meningitis may manifest in two forms:
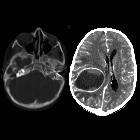
Leptomeningitis
TB leptomeningitis is common and presents with thick tuberculous exudate within the subarachnoid space, particularly pronounced at the base of the brain (especially in the interpeduncular fossa, anterior to the pons and around the cerebellum) and may also extend into the Sylvian fissures. In contrast to bacterial meningitis, extension over the surfaces of the cerebral hemispheres is relatively uncommon . Eventually, mass-like regions of caseous necrosis can form within this exudate, representing extra-axial tuberculomas.
Not surprisingly CSF flow is disrupted, and obstructive hydrocephalus is common.
An additional complication is arteritis that may result in ischemic infarcts, which are seen in approximately a third of cases, especially in children .
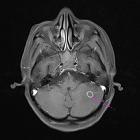
Pachymeningitis
In contrast, TB pachymeningitis is rare and is characterized by thick plaque-like regions of pachymeningeal enhancement. This term should be reserved for cases where it is an isolated abnormality, and not confused with the sometimes dramatic thickening of dura adjacent to a tuberculoma .
For further discussion please refer to separate articles on tuberculous leptomeningitis and tuberculous pachymeningitis.
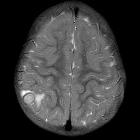
Tuberculoma
Intracranial tuberculomas may occur either in isolation or combined with extra-axial TB infection. They typically appear as ring-enhancing lesions with surrounding vasogenic edema. Centrally they tend to have only intermediate or even low signal on T2 weighted images (helpful in distinguishing them from the less common tuberculous abscess) . They may be associated with extensive adjacent leptomeningeal and/or pachymeningeal enhancement.
For further discussion, please refer to separate articles on intracranial tuberculoma.
Treatment and prognosis
Treatment of CNS tuberculosis is based on an anti-tubercular treatment regimen. However, multidrug-resistant tuberculosis remains a major hurdle in treatment.
Siehe auch:
- Meningeosis neoplastica
- Meningeom
- Hirnmetastase
- meningeale Kontrastmittelaufnahme
- Neurozystizerkose
- Neurosarkoidose
- Neurotoxoplasmose
- Erdheim-Chester-Erkrankung
- zerebrale Kryptokokkose
- ZNS Lymphom
- zerebrale Läsionen mit ringförmiger Kontrastmittelanreicherung
- Kleinhirnabszess
- Läsionen mit ringförmiger Kontrastmittelanreicherung
- bakterieller Hirnabszess
- Tuberkulom des ZNS
- tuberkulöse Meningitis
- zerebrale Miliartuberkulose
- ZNS-Manifestationen bei Langerhans-Zell-Histiozytose
- intrakranieller tuberkulöser Abszess
und weiter:
- Tuberkulose
- Basalganglienverkalkungen
- pulmonale Tuberkulose
- verdickter Hypophysenstiel
- Tuberkulose des ZNS
- Meningitis
- neuroradiologisches Curriculum
- tuberculoma
- primäre diffuse leptomeningeale Gliomatose (PDLG)
- extrapulmonale Manifestationen der Tuberkulose
- hypertrophe Pachymeningitis
- Tuberkulose der Wirbelsäule und des Spinalkanals
- Glioblastom mit leptomeningealen Metastasen
- cerebellar tuberculoma
- spinal tuberculous arachnoiditis
- granulomatöse Hypophysitis
- Lungentuberkulose und ZNS-Tuberkulose
- miliary cerebral tuberculosis
- hyperintense Meningen
- cerebellar tuberculomas
- pädiatrische zerebrale Infektionen
- Metastasen in der Hypophyse

 Assoziationen und Differentialdiagnosen zu Tuberkulose des ZNS:
Assoziationen und Differentialdiagnosen zu Tuberkulose des ZNS: