Lungensequester


























Pulmonary sequestration, also called accessory lung, refers to the aberrant formation of segmental lung tissue that has no connection with the bronchial tree or pulmonary arteries. It is a bronchopulmonary foregut malformation (BPFM).
There are two types:
- intralobar sequestration (ILS)
- extralobar sequestration (ELS)
- extralobar intrathoracic
- extralobar subdiaphragmatic
Epidemiology
The estimated incidence is 0.1%. Some authors propose a greater male prevalence (this may be the case for the extralobar type) . The age of presentation is dependent on the type of sequestration (see below).
Clinical presentation
Extralobar sequestration (ELS) more commonly presents in newborns as respiratory distress, cyanosis, or infection, whereas intralobar sequestration (ILS) presents in late childhood or adolescence with recurrent pulmonary infections.
Pathology
Pulmonary sequestration can be divided into two distinct groups based on the relationship of the aberrant segmental lung tissue to the pleura:
- intralobar sequestration (ILS)
- accounts for the majority (75-85% of all sequestrations )
- present later in childhood with recurrent infections
- extralobar sequestration (ELS)
- less common (15-25% of all sequestrations )
- usually present in the neonatal period with respiratory distress, cyanosis, or infection
- recognized male predilection M: F ratio ~4:1
- can be infradiaphragmatic in ~10% of cases
The two types of sequestration are similar in their relationship to the bronchial tree and arterial supply/venous drainage but differ in their relationship to the pleura.
By definition, there is no communication with the tracheobronchial tree. In the vast majority of cases, the abnormal lung tissue has a systemic arterial supply which is usually a branch of the aorta:
- intralobar sequestrations
- venous drainage commonly occurs via the pulmonary veins but can occur through the azygous-hemiazygous system, portal vein, right atrium or inferior vena cava
- closely connected to the adjacent normal lung and do not have a separate pleura
- extralobar sequestrations
- venous drainage most commonly through the systemic veins into the right atrium (but is variable)
- separated from any surrounding lung by its own pleura
Genetics
Almost all cases occur sporadically.
Location
Overall, sequestration preferentially affects the lower lobes. 60% of intralobar sequestrations affect the left lower lobe, and 40% the right lower lobe. Extralobar sequestrations almost always affect the left lower lobe, however, ~10% of extralobar sequestrations can be subdiaphragmatic .
Associations
Associated disease is common with the extralobar type (50-60%):
- congenital pulmonary airway malformation (CPAM): which is then sometimes termed a hybrid lesion
- congenital heart disease
- congenital diaphragmatic hernia
- Scimitar syndrome
Radiographic features
Plain radiograph
- often show a triangular opacity in the affected segment
- may show cystic spaces if infected
- both ILS and ELS can rarely have air bronchograms as they may acquire a connection to the bronchial tree due to an infective process or, rarely, they can have foregut communication (esophagus or stomach) as part of hybrid lesion
Ultrasound
The sequestrated portion of the lung is usually more echogenic than the rest of the lung. On antenatal ultrasound, an extralobar sequestration may be seen as early as 16 weeks gestation and typically appears as a solid well-defined triangular echogenic mass . Color Doppler may identify a feeding vessel (in-utero cases) from the aorta. If the sequestration is subdiaphragmatic, it may appear as an echogenic intra-abdominal mass.
CT
- cross-sectional imaging frequently demonstrates the arterial supply by the descending aorta
- they may arise below the diaphragm in 20% of patients
- usually does not contain air unless infected
- 3D reconstructions can be particularly helpful in detecting
- anomalous arterial vessels
- concurrent anomalous veins
- differentiating between intralobar and extralobar sequestrations
Angiography (DSA)
Not part of the routine investigation but is the gold standard in determining arterial supply.
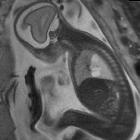
MRI
- T1: the sequestrated segment tends to be of comparatively high signal to normal lung tissue
- T2: also tends to be of comparatively high signal
- MRA: can be helpful in demonstrating anomalous arterial supply
Treatment and prognosis
Traditionally treatment has been surgical resection. Extralobar sequestrations with their separate pleural investments can usually be removed sparing normal lung tissue, although, with an intralobar type, segmental resection or even lobectomy will be necessary.
Coil embolization has also been successfully trialed in selected cases . Spontaneous involution has been reported in occasional cases .
Complications
- frequent respiratory tract infection
- in neonates can be complicated by high output cardiac failure
Differential diagnosis
General imaging differential considerations include:
- persistent pneumonia
- pulmonary abscess
- congenital pulmonary airway malformation (CPAM)
- can also be an association: bronchopulmonary foregut malformation hybrid lesion
- bronchogenic cyst
- can also be an association: bronchopulmonary foregut malformation hybrid lesion
- pulmonary arteriovenous malformation
- scimitar syndrome
- small lung with ipsilateral mediastinal shift
- tubular structure paralleling the right heart border in the shape of a Turkish sword (“scimitar”)
- right heart border may be blurred and may be mistaken by a triangular-shaped sequestration
- for anomalous systemic vessel without distinct sequestration consider anomalous systemic arterial supply to normal lung (also called Pryce type 1 sequestration)
- if with concurrent lung infection consider pulmonary pseudosequestration
Siehe auch:
- Bronchogene Zyste
- arteriovenöse Malformationen der Lunge
- kongenitale pulmonale Atemwegsmalformation (CPAM)
- Herzfehler
- Scimitar-Syndrom
- Lungensequester extralobulär
- kongenitale Zwerchfellhernie
- hybrid lesion: CCAM - pulmonary sequestration
- intralobar pulmonary sequestration
- kindliche Lungenläsionen
- bronchopulmonale Vordarmmalformation
und weiter:
- Pneumatozele
- Lungenvenenfehlmündung
- Neuroblastom
- Kavernöse Lungenläsionen
- Chylothorax
- Snowman heart
- fetal pleural effusion
- Unterlappenatelektase rechts
- pulmonary cavity (mnemonic)
- Duplikationszyste des Vorderdarms
- totale Lungenvenenfehlmündung
- partielle Lungenvenenfehlmündung
- neonatal chest radiograph in the exam setting
- echogenic fetal lung lesions
- pulmonary venolobar syndrome
- zystische Lungenläsionen bei Kindern
- cytic lung lesions - paediatric
- hybrid lesion : paediatric chest
- Acute Respiratory Distress Syndrome neonatal
- Zwerchfelldefekte
- Ursachen für Perfusionsdefekte in der Lungenventilations / -perfusionsszintigraphie
- intrapulmonale bronchogene Zyste
- Ösophagusduplikatur
- spontane Regression Lungensequester

 Assoziationen und Differentialdiagnosen zu Lungensequester:
Assoziationen und Differentialdiagnosen zu Lungensequester: