Pseudoaneurysms









































False aneurysms, also known as pseudoaneurysms, are abnormal outpouchings or dilatation of arteries which are bounded only by the tunica adventitia, the outermost layer of the arterial wall. These are distinguished from true aneurysms, which are bounded by all three layers of the arterial wall. Pseudoaneurysms typically occur when there is a breach in the vessel wall such that blood leaks through the inner wall but is contained by the adventitia or surrounding perivascular soft tissue.
Pathology
Etiology
- trauma (dissection or laceration)
- iatrogenic (dissection, laceration or puncture)
- arterial catheterization - accounts for most iatrogenic pseudoaneurysms
- biopsy, surgery
- spontaneous dissection
- fibromuscular dysplasia (dissection)
- mycotic aneurysm (inflammatory digestion of the vessel wall)
- myocardial infarction (left ventricular false aneurysm)
- regional inflammatory process
- vessel injury/erosion due to a tumor: relatively uncommon
- vasculitides
- penetrating atherosclerotic ulcer
Location
They can involve any arterial segment or even a cardiac chamber. Examples include
- aortic pseudoaneurysm: traumatic aortic pseudoaneurysm
- femoral artery pseudoaneurysm: relatively common site due to femoral punctures
- carotid artery pseudoaneurysm
- visceral arterial pseudoaneurysm
- hepatic arterial pseudoaneurysm
- gastroduodenal arterial pseudoaneurysm
- splenic arterial pseudoaneurysm
- peri-pancreatic pseudoaneurysm
- renal arterial pseudoaneurysm
- peripheral arterial (limb) pseudoaneurysm
- left ventricular pseudoaneurysm
- brachiocephalic artery pseudoaneurysm
Radiographic features
Some of the imaging features may be dependent on location.
Ultrasound
Due to the turbulent forward and backward flow, a characteristic yin-yang sign may be seen on color flow while a "to and fro" pattern may be seen with pulsed Doppler.
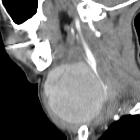
CT
- hypoattenuating (non-contrast) or hyperattenuating (contrast-enhanced) smooth-walled sac adjacent to an artery, usually with a communication
Treatment and prognosis
The risk of rupture is higher than that of a true aneurysm of comparable size due to poor support of the aneurysm wall and thus false aneurysms generally require treatment.
Siehe auch:
- penetrierendes Aortenulkus (PAU)
- Polyarteriitis nodosa
- Aneurysma
- Vaskulitis
- Fibromuskuläre Dysplasie
- systemischer Lupus Erythematodes
- Morbus Behçet
- Chronische Pankreatitis
- Akute Pankreatitis
- Takayasu-Arteriitis
- mykotisches (infiziertes) Aneurysma
- posttraumatisches Aneurysma spurium
- Riesenzellarteriitis
- femoral artery pseudoaneurysm
- true aneurysm
- Pseudoaneurysma des linken Ventrikels
- Pseudoaneurysma der Arteria iliaca
- management of pseudoaneurysm
- brachiocephalic artery pseudoaneurysm
- Pseudoaneurysma der Arteria carotis
- Pseudoaneurysma der Aorta
- pseudoaneurysm following blunt trauma
- yin-yang sign
und weiter:
- Ductus diverticulum
- Aneurysma der Arteria poplitea
- Aneurysma Aorta ascendens
- traumatic pseudoaneurysm
- Aneurysma spurium Arteria hepatica
- Pseudoaneurysma der Milzarterie
- pseudoaneurysm of the hepatic artery with associated arterio-portal fistula and hemobilia
- popliteal artery pseudoaneurysm associated with femoral exostosis
- thoracic aorta stent graft implantation - treatment of traumatic pseudoaneurysm
- popliteal artery pseudoaneurysm
- the yin-yang sign
- superselective embolisation of a post-radiotherapy false aneurysm of the maxillary artery
- pseudoaneurysm of the internal maxillary artery
- pseudoaneurysm of the peroneal artery
- post-surgical pseudoaneurysm in aortic coarctation
- post-radiotherapy false aneurysm
- Aneurysma spurium der Pulmonalarterien
- Aneurysma spurium der Koronararterien
- Dilatation der Aorta thoracica

 Assoziationen und Differentialdiagnosen zu Aneurysma spurium:
Assoziationen und Differentialdiagnosen zu Aneurysma spurium:












