leukodystrophy





The leukodystrophies are a heterogeneous group of disorders that primarily affect the white matter of the central nervous system. They are particularly encountered in childhood as many are genetically determined and represent abnormalities in white matter metabolism. A number of leukodystrophies can also, or rarely exclusively, present in adulthood; see adult-onset leukodystrophies.
Terminology
The term leukodystrophy is not, unfortunately, precisely defined and significant heterogeneity is encountered across publications as to which conditions are considered to be leukodystrophies.
For example, in some instances only genetically determined white matter disorders characterized by abnormal myelin formation (dysmyelinating disorders) are included, whereas others cast a wider net and also include those that are primarily due to abnormal breakdown of myelin (demyelinating disorders) and/or lack of normal myelination (hypomyelinating disorders).
Additionally, there is also overlap with other poorly defined terms such as leukoencephalopathy or even white matter diseases.
Be that as it may, there is a group of conditions that most would agree represent leukodystrophies, and it is this group that is presented immediately below in the "common and/or typical leukodystrophies" section.
Common and/or typical leukodystrophies
The following conditions are generally accepted as representing typical and/or common examples of leukodystrophies :
- Alexander disease
- Canavan disease
- globoid cell leukodystrophy (Krabbe disease)
- megalencephalic leukoencephalopathy with subcortical cysts
- metachromatic leukodystrophy
- Pelizaeus-Merzbacher disease
- vanishing white matter disease
- X-linked adrenoleukodystrophy
There are, however, a far larger number of conditions that are sometimes included in lists of leukodystrophies or more broadly genetically determined white matter disorders. These are presented below in the "Genetically-determined disease of white matter".
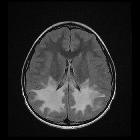
Radiographic features
The specific imaging features encountered widely between conditions and in some instances between individuals with the same condition. They are, therefore, discussed separately. There are, however, certain important concepts that are worth considering when reviewing imaging of an individual who possibly has a leukodystrophy, and these are presented below.
Before doing so, it is crucial to stress that even when imaging features are characteristic, a final diagnosis usually requires genetic testing .
- MRI is the modality of choice for assessing possible leukodystrophies
- symmetric involvement: this is generally true of the majority of leukodystrophies
- regional involvement: many leukodystrophies have a characteristic predilection for certain regions (e.g. X-linked adrenoleukodystrophy most commonly involves the occipitoparietal white matter)
- involvement or sparing of subcortical U-fibers
History and etymology
The word leukodystrophy means failure of white matter growth, derived from the Greek leuko meaning "white", dys meaning "abnormal", and trophos meaning "growth" or "nourishment" .
Genetically determined disease of white matter
There are very many genetically determined diseases that affect white matter and whether or not they are considered to be true leukodystrophies varies widely from publication to publication. Below is a classification adapted from one proposed in 2017 by van der Knaap and Bugiani and divides these genetically determined conditions according to what component of the white matter is primarily targetted. Naturally, this is merely one of many possible classifications and does not include all conditions that could be included in such a classification.
- astrocytopathies
- Aicardi-Goutières syndrome
- Alexander disease
- CIC-2-related disease
- giant axonal neuropathy
- megalencephalic leukoencephalopathy with subcortical cysts
- oculodentodigital dysplasia
- vanishing white matter disease
- leuko-axonopathies
- early-onset neuronal degenerative disorders
- GM1 and GM2 gangliosidoses (e.g. Tay Sachs disease)
- giant axonal neuropathy
- hypomyelination with atrophy of basal ganglia and cerebellum (H-ABC)
- hypomyelination with congenital cataract
- leukoencephalopathy with brainstem and spinal cord involvement and lactate elevation
- hypomyelination with brainstem and spinal cord involvement and leg spasticity
- Pol III-related leukodystrophies
- early-onset neuronal degenerative disorders
- leuko-vasculopathies
- CADASIL
- CARASIL
- cathepsin A-related arteriopathy with strokes and leukoencephalopathy
- cerebral amyloid angiopathy
- Fabry disease
- leukoencephalopathy with calcifications and cysts (Labrun syndrome)
- microgliopathies
- myelin disorders
- hypomyelination
- 18q-deletion syndrome
- fucosidosis
- Pelizaeus-Merzbacher disease
- Pelizaeus-Merzbacher-like disease 1
- demyelination
- myelin vacuolisation
- hypomyelination
- other
- adult-onset autosomal dominant leukodystrophy
- cerebrotendinous xanthomatosis
- cystic leukoencephalopathy without megalencephaly
- L-2-hydroxyglutaric aciduria
- lysosomal storage diseases
- free sialic acid storage disorders (e.g. Salla disease)
- Niemann-Pick disease
- peroxisomal disorders
- Sjögren-Larsson syndrome
Siehe auch:
- Morbus Fabry
- Leigh-Syndrom
- Mukopolysaccharidose
- Morbus Alexander
- Morbus Canavan
- Zellweger-Syndrom
- adrenoleukodystrophy
- Glutarylazidurie Typ 1
- Metachromatische Leukodystrophie
- Kearns-Sayre-Syndrom
- Pelizaeus Merzbacher disease
- Mitochondriale Encephalomyopathie mit Lactatacidose und Schlaganfall-ähnlichen Episoden (MELAS)
- dysmyelinating disease
- Neuropädiatrie Leitlinien Leukodystrophie
- DGN Leitlinien Leukodystrophie
- Globoidzellleukodystrophie
und weiter:

 Assoziationen und Differentialdiagnosen zu Leukodystrophie:
Assoziationen und Differentialdiagnosen zu Leukodystrophie:











