pulmonary embolism
















































Pulmonary embolism (PE) refers to embolic occlusion of the pulmonary arterial system. The majority of cases result from thrombotic occlusion, and therefore the condition is frequently termed pulmonary thromboembolism which is what this article mainly covers.
Other embolic sources include:
- air embolism
- carbon dioxide embolism
- other gas embolisms (e.g. nitrogen, helium)
- fat embolism
- tumor embolism: comprised of tumor thrombus
- hydatid embolism
- parasitic embolism
- talc embolism
- iodinated oil embolism
- metallic
- amniotic fluid embolism
- cement embolism: comprised of polymethyl methacrylate (PMMA)
- catheter embolism
- septic embolism
- brachytherapy seeds
Terminology
Classification of a pulmonary embolism may be based upon:
- the presence or absence of hemodynamic compromise
- temporal pattern of occurrence
- the presence or absence of symptoms
- the vessel which is occluded
Clinical presentation
The patient may report a history of recent immobilization or surgery, active malignancy, hormone usage, or a previous episode of thromboembolism. The physical exam may reveal suggestive features such as:
- clinical signs of deep venous thrombosis (DVT)
- asymmetric pitting lower extremity edema
- prominent superficial collateral vessels
- tenderness to palpation along the deep venous system
- tachycardia
- dyspnea
- pleuritic chest pain
- hemoptysis
Clinical decision rules, in conjunction with physician gestalt and estimated pretest probability of disease, may serve as a supplement in risk stratification:
ECG
- sinus tachycardia: the most common abnormality
- right heart strain pattern
- incomplete or complete right bundle branch block
- prominent R wave in lead V1
- right axis deviation
- T-wave inversion in the right precordial leads +/- the inferior leads is seen in up to 34% of patients and is associated with high pulmonary artery pressures
- simultaneous T-wave inversion in lead III and V1 has been repeatedly shown to have strong sensitivity (90%), specificity (97%), positive predictive value (92%), negative predictive value (96%) and overall predictive accuracy of 95%
- SIQIIITIII pattern: this refers to a deep S wave in lead I, Q wave and T wave inversion in lead III; this sign is seen as classical of PE but is, in fact, poor in terms of both sensitivity and specificity as a sign of PE
Pathology
Risk factors
- primary hypercoagulable states
- recent surgery
- prolonged bed rest/immobility
- malignancy: including multiple myeloma
- HIV :
- 2-10 x increased risk, cf. non-HIV matched controls
- COVID-19
- oral contraceptive use
- pregnancy
- known or previous DVT
- presence of certain venous aneurysms
Markers
D-dimer (ELISA) is commonly used as a screening test in patients with a low and moderate probability clinical assessment, on these patients:
- normal D-dimer has almost 100% negative predictive value (virtually excludes PE): no further testing is required
- raised D-dimer is seen with PE but has many other causes and is, therefore, non-specific: it indicates the need for further testing if pulmonary embolism is suspected
In patients with a high probability clinical assessment, a D-dimer test is not helpful because a negative D-dimer result does not exclude pulmonary embolism in more than 15%. Patients are treated with anticoagulants while awaiting the outcome of diagnostic tests .
Classification
- hemodynamic
- massive PE
- submassive PE
- low-risk
- temporal pattern
- acute
- subacute
- chronic
- vessel
- saddle
- lobar
- segmental
- subsegmental
Radiographic features
Depends to some extent on whether it is acute or chronic. Overall, there is a predilection for the lower lobes.
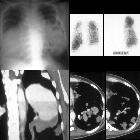
Plain radiograph
Chest radiography is neither sensitive nor specific for a pulmonary embolism. It is used to assess for differential diagnostic possibilities such as pneumonia and pneumothorax rather than for the direct diagnosis of PE.
Described chest radiographic signs include:
- Fleischner sign: enlarged pulmonary artery (20%)
- Hampton hump: peripheral wedge of airspace opacity and implies lung infarction (20%)
- Westermark sign: regional oligemia and highest positive predictive value (10%)
- pleural effusion (35%)
- knuckle sign
- Palla sign : enlarged right descending pulmonary artery
- Chang sign : dilated right descending pulmonary artery with sudden cut-off
Sensitivity and specificity of chest x-ray signs :
- Westermark sign
- sensitivity: ~14%
- specificity: ~92%
- positive predictive value: ~38%
- negative predictive value: ~76%
- vascular redistribution
- sensitivity: ~10%
- specificity: ~87%
- positive predictive value: ~21%
- negative predictive value: ~74%
- Hampton hump
- sensitivity: ~22%
- specificity: ~82%
- positive predictive value: ~29%
- negative predictive value: ~76%
- pleural effusion
- sensitivity: ~36%
- specificity: ~70%
- positive predictive value: ~28%
- negative predictive value: ~76%
- elevated diaphragm
- sensitivity: ~20%
- specificity: ~85%
- positive predictive value: ~30%
- negative predictive value: ~76%
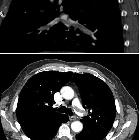
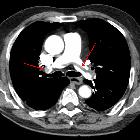
CT
Acute pulmonary emboli
CT pulmonary angiography (CTPA) will show filling defects within the pulmonary vasculature with acute pulmonary emboli. When the artery is viewed in its axial plane the central filling defect from the thrombus is surrounded by a thin rim of contrast, which has been called the Polo Mint sign.
Emboli may be occlusive or non-occlusive, the latter is seen with a thin stream of contrast adjacent to the embolus. Typically the embolus makes an acute angle with the vessel, in contrast to chronic emboli. The affected vessel may also enlarge .
Acute pulmonary thromboemboli can rarely be detected on non-contrast chest CT as intraluminal hyperdensities .
Dual-energy CT holds much promise for the diagnosis and prognosis of PE.
Chronic pulmonary emboli
In contrast to acute pulmonary embolism, chronic thromboemboli are often complete occlusions or non-occlusive filling defects in the periphery of the affected vessel which form obtuse angles with the vessel wall . The thrombus may be calcified.
Features noted with chronic pulmonary emboli include:
- webs or bands, intimal irregularities
- abrupt narrowing or complete obstruction of the pulmonary arteries
- “pouching defects” which are defined as chronic thromboembolism organized in a concave shape that “points” toward the vessel lumen
Indirect signs include :
- mosaic perfusion
- vascular calcification
- bronchial or systemic collateralisation
Ultrasound/Echocardiography
Acute pulmonary emboli
Point-of-care ultrasonography is currently not recommended for a haemodynamically stable patient with suspected pulmonary embolism. In the presence of hemodynamic compromise, echocardiography may be of value to assess for the presence of severe right ventricular dysfunction;
- if absent, another cardiopulmonary derangement is likely responsible
- if unequivocally present, it can establish the need for emergent treatment
Echocardiographic features which may be suggestive include:
- thrombus-in-transit
- right ventricular dysfunction
- commonly dilated and hypocontractile
- flattening or dyskinesis of the interventricular septum
- 60/60 sign
- McConnell sign
Of note, transesophageal echocardiography has a reported sensitivity of 80.5% and a specificity of 97.2% for ruling in acute pulmonary embolism after the detection of right ventricular overload on transthoracic echocardiography .
Chronic pulmonary emboli
Again not recommended as part of first-line work up.
Cumulative damage from repeated embolic insults is a common cause of chronic thromboembolic pulmonary hypertension, which demonstrates a variable degree of the aforementioned signs, but with significantly higher right ventricular pressures, right ventricular hypertrophy and diastolic dysfunction, and a higher degree of tricuspid regurgitation.
MRI
It is difficult to obtain technically adequate images for pulmonary embolism patients using MRI. Magnetic resonance pulmonary angiography (MRPA) should be considered only at centers that routinely perform it well and only for patients for whom standard tests are contraindicated. Technically-adequate magnetic resonance angiography has a sensitivity of 78% and a specificity of 99% .
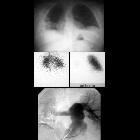
Nuclear medicine
A ventilation/perfusion (V/Q) scan will show ventilation-perfusion mismatches. A high probability scan is defined as showing two or more unmatched segmental perfusion defects according to the PIOPED criteria.
Treatment and prognosis
Providing cardiopulmonary support is the initial treatment. Anticoagulation is provided in patients without risk of active bleeding. If the emboli are large or there is a large clot burden, thrombolysis is an option. In some cases, embolectomy or placement of vena cava filters is required.
The right ventricular failure due to pressure overload is considered the primary cause of death in severe PE .
Complications
- acute emboli
- pulseless electrical activity (PEA) in the context of a large obstructing saddle embolus (see mnemonic for causes of PEA)
- acute or chronic emboli
- right ventricular dysfunction
- CT features suggestive of right ventricular dysfunction include :
- abnormal position of the interventricular septum
- inferior vena cava contrast reflux
- RVD (right ventricular diameter): LVD (left ventricular diameter) ratio >1 on reconstructed four-chamber views
- RVD:LVD ratio >1 on standard axial views is not considered to be a good predictor of right ventricular dysfunction
- termed submassive PE when right ventricular dysfunction demonstrated on imaging (CT or echo) but without clinical hemodynamic compromise
- CT features suggestive of right ventricular dysfunction include :
- right ventricular dysfunction
- subacute-to-chronic emboli
- pulmonary infarction
- pulmonary hypertension
- pulmonary arterial sclerosis
- chronic emboli
Resolution over time
Several studies report around 80% emboli resolving at around 30 days . According to one study, residual pulmonary obstruction at 6 months after the first episode of pulmonary embolism was shown to be an independent predictor of recurrent venous thromboembolism and/or chronic thromboembolic pulmonary hypertension .
Differential diagnosis
Consider:
- pulmonary artery sarcoma
- pulmonary artery vasculitis e.g. Takayasu arteritis
- misidentification of pulmonary veins for arteries
- arterial bifurcations (or branch points) can mimic PE but usually easily distinguished on multiplanar assessment
- artifact may cause pseudo-filling defects and can be caused by:
- breathing motion
- beam hardening
- hyperconcentrated contrast in the superior vena cava
- medical devices e.g. catheters, orthopedic prostheses
- patient's arms in a down position
- patient movement
- transient contrast bolus interruption , due to Valsalva or a patent foramen ovale, causing non-opacified blood to enter the right ventricle and pulmonary arteries (scanning in end-expiration can reduce or eliminate this artifact)
- chronic emboli may be mistaken for acute emboli
- or vice-versa
- thromboembolic emboli may be mistaken for other embolized material
- or vice-versa
See also

 Assoziationen und Differentialdiagnosen zu Lungenarterienembolie:
Assoziationen und Differentialdiagnosen zu Lungenarterienembolie: