intrakranielle Verkalkungen

Ausgeprägte,
zirkuläre Verkalkungen der A. carotis interna im kavernösen Verlauf. Computertomografie axial, koronar und sagittal jeweils im Knochenfenster.



Subdural
hemorrhage • Chronic calcified subdural hemorrhages - Ganzer Fall bei Radiopaedia

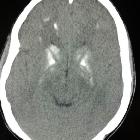
Severe
congenital cytomegalovirus infection due to maternal reinfection. Axial images reveal ventriculomegaly (*) and multiple periventricular calcifications (arrow).

Brain stones
revisited—between a rock and a hard place. A 17-year-old female with seizures presented with a large calcified mass apparently arising from the left temporal lobe. The calcification pattern (mostly peripheral) and morphology (“popcorn appearance”) strongly suggested a vascular lesion such as a cavernous malformation (cavernous angioma) or, less likely, a calcified haemangioma. Upon excision, the mass was later found to be a choroid plexus papilloma, shown in the axial NCECT in soft tissue (a) and bone windows (b) as well as the coronal NCECT reconstruction in soft tissue (c) and bone windows (d)

Multiple
intracranial calcifications • Giant cerebral arteriovenous malformation - Ganzer Fall bei Radiopaedia

This image
is part of a series which can be scrolled interactively with the mousewheel or mouse dragging. This is done by using Template:Imagestack. The series is found in the category Morbus Fahr case 002. Morbus Fahr in der Computertomographie. Ausgeprägte Verkalkungen in den Stammganglien und im Kleinhirn.

Brain stones
revisited—between a rock and a hard place. A 68-year-old male with transient right-sided hemiparesis. This preoperative NCECT was done following discovery of suspicious lesions from a recent MRI (not available). Axial (a), sagittal (b) and 3D reconstruction (c) show a calcified lesion (black arrows) in the left post central gyrus. The entire lesion was surgically removed and was found to be a glioblastoma with an extensive oligodendroglioma component. Ninety percent of oligodendrogliomas are known to form dense, clump-like calcifications

Brain stones
revisited—between a rock and a hard place. An 8-year-old male with a long complicated medical history was found to have hard-to-miss calcifications on the plain skull x-ray (a, d). The NCECT (b, e) and 3D reconstructions (c, f) show a large amorphous calcification originating from the basal ganglia, extending into the right lateral ventricle of the patient diagnosed with tuberous sclerosis. Subependymal nodules associated with tuberous sclerosis can calcify with age, typically presenting with globular or sometimes ring-like calcification

Brain stones
revisited—between a rock and a hard place. A 60-year-old male known HIV patient presented with seizures. The solid calcifications on NCECT at the right frontal (a) left basal ganglia (b) and right parietal areas (c) represent sequela following treatment for documented toxoplasmosis. 3D reconstruction (d). In congenital toxoplasmosis, calcifications have been shown to decrease in size or even completely resolve with treatment

Brain stones
revisited—between a rock and a hard place. Axial CT in bone windows (a) and 3D reconstruction (b) of a 33-year-old male with temporal lobe epilepsy. The large amorphous calcification seen at the base of the left temporal lobe in this NCECT represents a known case of an embolised AV malformation. Calcifications are known to appear in 25–30 % of cases in close conjuction with serpentine vessels or within adjacent brain parenchyma

Brain stones
revisited—between a rock and a hard place. Dystrophic calcification in a 73-year-old female with a prior history of intracranial bleed who presented with loss of consciousness. The NCECT scan (a), close-up view (b) and 3D reconstruction (c) showed “brain stones” (black arrows) in the middle of the pathological brain regions. There is also an intraventricular drain present (white arrows). The subsequent appearance of calcifications in known post-traumatic or post-ischaemic areas of the brain is largely attributed to dystrophic calcification

Brain stones
revisited—between a rock and a hard place. A 59-year-old female with back pain and an abnormal bone scan that showed a focal lesion in the skull. The faint calcification seen at the lateral skull x-ray (a) was confirmed on non-contrast-enhanced CT (NCECT) to be a calcified meningioma overlying the right frontal cortex (b), better visualised on the 3D reconstruction (c). Note the displacement of adjacent brain parenchyma (“cortical buckling”), which strongly suggests the extra-axial location of this lesion


Brain stones
revisited—between a rock and a hard place. Dural osteoma. A 53-year-old female who presented with a headache and distant history of head trauma. The FLAIR (a) and MIP-SWI (b) MRI sequences showed an area of signal loss (white arrows) in the right temporal lobe initially thought to represent an enlarged post-traumatic air cell. Subsequent NCECT (c) and 3D reconstruction (d) revealed a solid calcified lesion (black arrow) adherent to the squamous part of the temporal bone. Note the cortical buckling (a), which suggests an extra-axial location. The homogeneously solid calcification (c) suggests a dural osteoma instead of a dural ossification

Severe
congenital cytomegalovirus infection due to maternal reinfection. Axial (a-c), coronal (d-f) and sagittal (g-i) T2-weighted images show ventriculomegaly (*), ventricular adhesions (arrowhead), periventricular calcifications (open arrow), cystic lesions (thin arrow), diffuse white matter disease (thick arrow).

CT (without
contrast) of the brain of a 20 month old child with Sturge-Weber syndrome demonstrating prominent subcortical white matter calcification. The entire case (including MRI images can be seen at Radiopaedia.org here.

Brain stones
revisited—between a rock and a hard place. A 35-year-old female with a history of multiple shunt revisions was found to have symmetric calcifications in the cerebellum and basal ganglia on CT (a, b) and 3D reconstruction (c). Although not confirmed in this patient, the presence of symmetric calcifications in these regions in young patients is generally thought to be related to a possible diagnosis of Fahr syndrome or an endocrine disorder

Multiple
intracranial calcifications • Neurocysticercosis - Ganzer Fall bei Radiopaedia

Multiple
intracranial calcifications • Fahr disease - Ganzer Fall bei Radiopaedia

Multiple
intracranial calcifications • Pseudohypoparathyroidism - Ganzer Fall bei Radiopaedia

Multiple
intracranial calcifications • Mineralizing microangiopathy - Ganzer Fall bei Radiopaedia

Multiple
intracranial calcifications • Sturge-Weber syndrome - Ganzer Fall bei Radiopaedia

Central
nervous system germinoma • Pineal tumor calcification (illustration) - Ganzer Fall bei Radiopaedia

Cluster of
teeth in brain - Pituitary teratoma an uncommon tumor in common location. CT Brain bone window sagittal image showing a mass with a cluster of teeth like structures in sella and supra-sellar region. Sella is widened with no evidence of cortical erosion/ destruction.

This image
is part of a series which can be scrolled interactively with the mousewheel or mouse dragging. This is done by using Template:Imagestack. The series is found in the category Morbus Fahr case 001. Computertomographie des Schädels (ohne Kontrastmittel) bei einem Patienten mit Morbus Fahr. Man erkennt deutlich die ausgedehnten Verkalkungen in den Stammganglien und im Kleinhirn. Gleichzeitig findet sich ein Makroadenom der Hypophyse.
Intracranial calcifications are common in certain locations and often are of no clinical concern.
The two most commonly encountered types of calcification include:
Concerning calcifications are much less common and occur in a variety of settings, including
- infection
- metabolic
- previous cerebral insult
- healed cerebral abscess
- healed infarct
- healed hematoma
- vascular malformation
- radiation
- neurodegeneration
In these cases it is also important to exclude normal calcifications.
Siehe auch:
- Arteria carotis interna
- zerebrale Verkalkungen
- Morbus Fahr
- Arteria vertebralis
- Hirnabszess
- Neurozystizerkose
- Sturge-Weber-Krabbe-Syndrom
- zerebrale arteriovenöse Malformation
- Neurotoxoplasmose
- Sinus cavernosus
- Bochdalek-Blumenkörbchen
- Morbus Hippel-Lindau
- haematoma
- TORCH
- Pseudohypoparathyreoidismus
- mineralisierende Mikroangiopathie
- metastatic calcification in the brain
- normale intrakranielle Verkalkungen
- Eisenablagerungen im Gehirn
- cerebral coccidiomycosis
- Hypoparathyreoidismus
- intramurales Hämatom der Aorta
- intrakranielle Arteriosklerose
- Verkalkungen Kleinhirn
und weiter:
- verkalktes Corpus pineale
- congenital infections (mnemonic)
- fetal toxoplasmosis
- lymphoma vs toxoplasmosis
- tentorium cerebelli calcifications
- Occipitale Verkalkungen
- intrakranielle Arteriosklerose Säugling
- intrakranielle Verkalkungen in einem Parenchymschaden
- intrakranielles Chondrosarkom
- durales Chondrosarkom

 Assoziationen und Differentialdiagnosen zu intrakranielle Verkalkungen:
Assoziationen und Differentialdiagnosen zu intrakranielle Verkalkungen: