tuberculous leptomeningitis
















Tuberculous meningitis is the most common presentation of intracranial tuberculosis, and usually refers to infection of the leptomeninges. Uncommonly tuberculosis can be limited to the pachymeninges (dura mater), it is called tuberculous pachymeningitis and is discussed separately.
The remainder of this article pertains to leptomeningeal tuberculosis, which involves the arachnoid mater and pia mater.
Epidemiology
Tuberculous meningitis, although seen in all age groups, has a peak incidence in childhood (particularly 0-4 years of age) in high prevalence areas. In low prevalence areas, it is more frequently encountered in adolescents and adults.
Important risk factors include:
- HIV/AIDS
- immunosuppression
- diabetes mellitus
- alcoholism
Clinical presentation
Low-grade fever with headache is a prodromal manifestation. Most common clinical manifestations are fever, headache, vomiting and neck stiffness. Cranial nerve palsies of 3, 4 and 6nerves may be seen. Seizures, focal neurological deficits, stupor and coma may be seen in late stages.
CSF analysis reveals lymphocytosis, increased protein level and decreased glucose levels.
Pathology
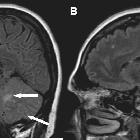
Tuberculous meningitis is caused by Mycobacterium tuberculosis. The infection spreads hematogenously from a distant focal point, usually pulmonary tuberculosis and lodges immediately deep to the pia forming Rich foci. These can rupture into the subarachnoid space, forming an exudate. This purulent material is primarily located in the vicinity of basal cisterns: inferomedial surface of frontal lobe, anteromedial surface of temporal lobes, superior cerebellum and floor of the fourth ventricle.
From here, infection spreads to interpeduncular cisterns, around optic chiasm and to pontomesencephalic, ambient and suprasellar cisterns. Although the exudate can reach the Sylvian fissures it uncommonly extends over the cerebral convexities .
Choroid plexitis may also be a late manifestation as is mass-like regions of caseous necrosis within this exudate.
Radiographic features
CT
- non-contrast scans may be normal
- later complications may be visible including:
- hydrocephalus
- infarcts due to arteritis (especially in children)
Following contrast administration a number of additional features may be visible:
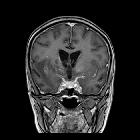
- basal enhancing exudates
- leptomeningeal enhancement, along sylvian fissures, tentorium uncommonly convexities
- ependymitis may be present
MRI
- T1
- normal initially
- T1 shortening may be seen after progression of disease
- T2
- normal initially
- T2 shortening is seen after disease progression
- T1 C+ (Gd): diffuse basal enhancement with enhancing exudates
- magnetization transfer (MT) spin echo: significantly lower MT ratio is seen in tuberculous meningitis as compared to fungal and pyogenic meningitis
Treatment and prognosis
Anti-tuberculosis regimen is started after confirmation of diagnosis. Treatment of complications (e.g. drainage of hydrocephalus) is also performed.
Complications
- hydrocephalus
- arteritis that may result in ischemic infarcts
- affects one-third of cases
- more common in children
- cranial neuropathies: most affected nerves are 3, 4 and 6 nerves
Differential diagnosis
General imaging differential considerations include:
- pyogenic meningitis
- leptomeningeal carcinomatosis
- disseminated oligodendroglial-like leptomeningeal tumor of childhood
- fungal meningitis
- neurosarcoidosis
Siehe auch:
- Tuberkulose
- Meningeosis neoplastica
- Cerebellum
- pulmonale Tuberkulose
- Chiasma opticum
- Tuberkulose des ZNS
- vierter Ventrikel
- Verschlusshydrocephalus
- tuberkulöse Pachymeningitis
- suprasellar cisterns
- interpeduncular cisterns
und weiter:
- meningeale Kontrastmittelaufnahme
- Subarachnoidalblutung
- Neurosarkoidose
- Meningitis
- leptomeningeale Kontrastmittelanreicherungen
- Moyamoya-Erkrankung
- extrapulmonale Manifestationen der Tuberkulose
- spinale Meningeosis neoplastica
- bakterielle Meningitis
- Moyamoya-Muster
- Meningitis CCT
- Tuberkulom des ZNS
- spinal tuberculous arachnoiditis
- leptomeningeal tuberculosis

 Assoziationen und Differentialdiagnosen zu tuberkulöse Meningitis:
Assoziationen und Differentialdiagnosen zu tuberkulöse Meningitis:








