orbital inflammatory syndrome



















Idiopathic orbital inflammation (IOI), also known as orbital pseudotumor and non-specific orbital inflammation, is an idiopathic inflammatory condition that most commonly involves the extraocular muscles. Less commonly there is inflammatory change involving the uvea, sclera, lacrimal gland, and retrobulbar soft tissue.
The exact etiology is not known but an association with many inflammatory/autoimmune diseases is reported.
Terminology
Many terms are used interchangeably in the literature to refer to idiopathic orbital inflammation including orbital pseudotumor, non-specific orbital inflammation and orbital inflammatory syndrome.
Clinical presentation
Patients typically present with rapid-onset, usually unilateral (~90% of cases), painful proptosis and diplopia. Idiopathic orbital inflammation is a diagnosis of exclusion; atypical presentation, poor response to treatment with corticosteroid and recurrence should prompt biopsy to exclude other diseases.
Pathology
Histologically acute lesions demonstrate lymphocytes (which can be mistaken for orbital lymphoma), plasma cells, and giant cell infiltration.
Classification
Division into a number of subgroups according to location has been proposed:
Associations
The condition has been associated with other inflammatory and autoimmune conditions:
- IgG4-related disease, now recognized as a separate entity: IgG4-related orbital disease
- sarcoidosis
- granulomatosis with polyangiitis
- systemic lupus erythematosus (SLE)
- polyarteritis nodosa (PAN)
- dermatomyositis
- rheumatoid arthritis (RA)
- sclerosing cholangitis
- Riedel thyroiditis
- mediastinal fibrosis
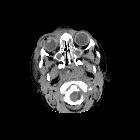
Radiographic features
Imaging demonstrates enlargement of the muscle belly of one (or more) extraocular muscles typically with the involvement of their tendinous insertions. Involvement of the tendinous insertion distinguishes it from thyroid-associated orbitopathy (TAO) in which the insertion point is spared. However, sparing of the anterior tendon does not preclude the diagnosis of idiopathic orbital myositis .
Additional inflammation can be seen in surrounding tissues, including the orbital fat, lacrimal gland, and optic nerve sheath.
It can appear as an infiltrative mass and extends outside of the orbit via superior or inferior orbital fissures. Extension into the cavernous sinus, meninges, and dura can occur. It is most commonly unilateral but can be bilateral in 25% of cases.
MRI
Reported signal characteristics include:
- T1: affected region typically isointense (to extra-ocular muscles) but can also be hypointense
- T2: affected region typically hypointense due to fibrosis and with more progression of fibrosis it becomes more hypointense, but the signal can also be iso- to hyperintense to extra-ocular muscles
- T1 C+ (Gd): moderate to a marked diffuse enhancement
Treatment and prognosis
Most cases resolve rapidly with treatment (usually corticosteroids suffice) although in a subset with more chronic progression chemotherapy and radiotherapy may be required. A degree of residual fibrosis can be demonstrated, especially in the more refractory cases.
History and etymology
The disease was first described by Birch-Hirschfeld et al. in 1905 . They also introduced the term orbital pseudotumor afterward in 1930 .
Differential diagnosis
One of the main differential diagnoses of idiopathic orbital inflammation is orbital lymphoma. There is considerable overlap between these entities both clinically and radiologically. However, orbital lymphoma usually presents as a progressive orbitopathy rather than acutely, is more often bilateral, shows lower values on ADC, and does not respond to corticosteroid.
Other imaging differential considerations include:
- orbital cellulitis: usually associated with a subperiosteal abscess from adjacent sinusitis or with a previous history of trauma/dental procedure
- thyroid-associated orbitopathy (TAO): spares the tendinous insertions and not usually painful
- Tolosa-Hunt syndrome: related condition with the involvement of the cranial nerves in the cavernous sinus and resulting ophthalmoplegia
- granulomatosis with polyangiitis: bilateral involvement of the paranasal sinuses and orbits associated with osseous destruction
- orbital sarcoidosis
- orbital metastases
- orbital rhabdomyosarcoma
Siehe auch:
- Polyarteriitis nodosa
- Rheumatoide Arthritis
- intraorbitale Raumforderungen
- Granulomatose mit Polyangiitis
- Dermatomyositis
- orbitales Lymphom
- systemischer Lupus Erythematodes
- Exophthalmus
- Metastasen in der Orbita
- Orbitaphlegmone
- inflammatorischer Pseudotumor
- Rhabdomyosarkom der Orbita
- sclerosing cholangitis
- fibrosierende Mediastinitis
- Graves ophthalmopathy
- Riedel-Thyreoiditis
- idiopathic orbital myositis
- Sarkoidose der Glandula ladrimalis
- retroperitoneale Fibrose allgemein
- Unterscheidung inflammatorischer Pseudotumor der Orbita und orbitales Lymphom
- Orbitaspitzensyndrom
- Entzündungen der Glandula ladrimalis
und weiter:
- Meningeom Nervus opticus
- dysthyroid eye disease
- orbital pathology
- tram-track sign
- plasma cell granuloma
- intraokulare Raumforderungen
- Pseudotumor
- Orbita
- rhabdomyosarcoma of the orbit
- verdickter Nervus Opticus
- inflammatorischer Pseudotumor der Schädelbasis
- orbital myositis
- Tuberkulose der Orbita
- Adenokarzinom der Glandula lacrimalis

 Assoziationen und Differentialdiagnosen zu inflammatorischer Pseudotumor der Orbita:
Assoziationen und Differentialdiagnosen zu inflammatorischer Pseudotumor der Orbita: