hepatic metastasis




























Hepatic metastases are 18-40 times more common than primary liver tumors . Ultrasound, CT, and MRI are all useful for detection of hepatic metastases and evaluation across multiple post-contrast CT series, or MRI pulse sequences are necessary.
Epidemiology
The demographics of patients with liver metastases will mirror that of the underlying primaries. Incidence, therefore, increases with age.
Clinical presentation
Liver metastases are usually asymptomatic and found during workup of a malignancy which has presented in other ways. If the hepatic metastatic burden is large then the presentation or symptoms related to the liver disease may include:
- localized pain and tenderness due to capsular stretching
- disordered liver metabolic function
- ascites
- low-grade fever
Pathology
The most common sites of primary malignancy that metastasize to the liver are :
- gastrointestinal tract (via portal circulation)
- breast cancer
- lung cancer
- genitourinary system
- melanoma
- sarcomas
- adrenocortical carcinomas
- essentially all metastatic solid malignancies
- testicular cancer
Radiographic features
One of the main difficulties in liver imaging for metastatic disease is the high prevalence of benign liver lesions that can be misinterpreted as evidence of metastatic disease, thus dramatically changing a patients stage, and therefore treatment options. Liver hemangiomas, and to a lesser degree focal nodular hyperplasia (FNH), are the main sources of confusion . Additionally, pseudolesions (e.g. transient hepatic attenuation differences (THADs), focal fatty sparing / focal fatty change) may further muddy the waters. Therefore, an understanding of the various appearances of metastatic disease is crucial.
Ultrasound
Routine greyscale ultrasound, contrast-enhanced ultrasound, and intra-operative ultrasound all have roles to play.
Unfortunately, not only do metastases have a wide range of appearances, but background echogenicity changes of the liver due to fatty change make absolute statements difficult to make. In general, however, metastases may appear as :
- rounded and well defined
- positive mass effect with distortion of adjacent vessels
- hypoechoic: most common ~65% and is a concerning feature
- hypoechoic halo due to compressed and fat spared liver
- cystic, calcified, infiltrative and echogenic appearances are all possible: see liver metastases ultrasound appearances
Contrast-enhanced ultrasound has similar characteristics to CT, able to distinguish between hypovascular liver lesions, and hypervascular liver lesions.
See also: ultrasound appearance of hepatic metastases.
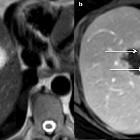
CT
Liver metastases are typically hypoattenuating on unenhanced CT, enhancing less than surrounding liver following contrast . If there is concomitant hepatic steatosis, then the lesions may be iso- or even slightly hyperattenuating. Enhancement is typically peripheral, and although there may be central filling in, on portal venous phase, the delayed phase will show washout; helpful in distinguishing a metastasis from a hemangioma .
Some primaries have a tendency to produce hyper-enhancing metastases, including renal cell carcinoma, thyroid carcinoma, neuroendocrine tumors, etc (see hypervascular liver lesions).
MRI
The appearance of liver metastases on MRI is also variable, but MRI is more sensitive than CT for the detection of liver metastases . MRI examination of the liver may involve numerous sequences (see liver MRI protocol), and choice of the gadolinium contrast agent (extracellular contrast agent or Eovist) is an important consideration.
Most frequent appearances are :
- T1: moderately hypointense
- T2: mildly to moderately hyperintense
- T1 C+ (Gd): enhancement may be lesional or perilesional (enhancement outside the confines of the T1 delineated lesion)
- small lesions (<1.5 cm) tend to uniformly enhance.
- larger lesions (>1.5 cm) tend to show transient rim enhancement (i.e. with wash-out); helpful feature in distinguishing a metastasis from a liver hemangioma
- perilesional enhancement is most commonly seen in colorectal and pancreatic adenocarcinoma metastases
- T1 C+ (Eovist):
- Eovist is often useful for detection and confirmation of metastatic disease
- on the delayed phase, metastatic lesion do not retain any Eovist and essentially appear as "holes" in the liver
Fluid-fluid levels are considered a specific finding for neuroendocrine tumor metastases .
Treatment and prognosis
Hepatic metastases from colorectal adenocarcinoma can potentially be treated with hepatic metastasectomy, since they may be the only site of metastatic disease. Up to 20% of patients undergoing metastasectomy for this indication remain disease-free . Multiple staging systems for disease-free survival after metastasectomy have been proposed and are being refined. One of the more frequently used systems (Clinical risk score (CRS), "Fong" score) includes variables such as :
- node-negative primary
- single hepatic metastasis
- hepatic metastasis size <5 cm
- CEA <200 ng/mL
- disease-free interval >1 year
These variables suggest a better metastasectomy disease-free survival.
Transarterial chemotherapy and radioembolization are other options for treatment for hepatic metastases. MRI guided adaptive radiation therapy is a new and unique method of liver tumor treatment for both primary and metastatic disease .
Differential diagnosis
General differential imaging considerations include:
- hepatic hemangioma: usually hyperechoic, geographic, no mass effect, discontinuous peripheral nodular enhancement and 'filling in'
- multiple hepatic cysts: no enhancement or mural nodules; can be hyper-dense/intense due to blood or infection
- hepatocellular carcinoma (HCC): hypervascular, more often solitary, possible hypoechoic US halo, cirrhotic liver, vascular invasion
- focal nodular hyperplasia (FNH)
- often younger patients
- central scar, with persistent delayed enhancement
- hepatic adenoma
- transient hepatic attenuation differences (THAD): often in cirrhosis
- multifocal fatty infiltration/focal fatty sparing: periligamentous, perivascular distribution; MRI in-out phase signal changes, vessels course through "lesions"; no mass effect
- multiple biliary hamartomas
- cholangiocarcinoma: delayed enhancement, capsular retraction
- multiple liver abscesses: possible CT cluster sign and right pleural effusion
- hepatic peliosis
- primary non-Hodgkin lymphoma
Siehe auch:
- Leberhämangiom
- Leberzirrhose
- hepatozelluläres Karzinom
- Leberabszess
- Leberadenom
- Von-Meyenburg-Komplex
- Fokale noduläre Hyperplasie
- fokale Leberverfettung
- fokale Minderverfettung der Leber
- zystische Lebermetastasen
- simple Leberzyste
- Peliosis hepatis
- Lebermetastasen bei Mammakarzinom
- Lebermetastasen bei Magenkarzinom
- transient hepatic attenuation differences (THAD)
und weiter:
- hypodense Leberläsionen
- hypervaskularisierte Leberläsionen
- Echinococcus Leber
- Hepatoblastom
- cholangiozelluläres Karzinom
- ultrasound appearances of liver metastases
- Differenzialdiagnosen zystischer Leberläsionen
- echoreiche Leberherde
- multifokale noduläre Steatosis hepatis
- sonographic halo sign
- Metastasenleber
- Organmetastasen
- fibrolamelläres hepatozelluläres Karzinom
- embolisation of liver tumors
- hypervascular hepatic metastases
- Transarterielle Chemoembolisation
- fibrolamelläres Leberkarzinom im Kindesalter
- Pseudozirrhose der Leber
- Abszess durch Escherichia coli
- Lebermetastasen Pankreaskarzinom
- Lebermetastasen bei Kolonkarzinom
- liver metastases from a sacral chordoma
- target sign liver metastases
- accurate measurements using a new algorithm in a patient with hepatic metastases from colon cancer
- Lebermetastasen bei Dünndarmkarzinom CT
- Lebermetastasen neuroendokriner Tumoren
- CUP hepatic metastases
- multiple hypodense Leberherde
- liver metastases from lung cancer
- Lebermetastasen Wilmstumor
- Metastasen Gallenblasenkarzinom

 Assoziationen und Differentialdiagnosen zu Lebermetastasen:
Assoziationen und Differentialdiagnosen zu Lebermetastasen: