cerebellar abscess






































Brain abscess is a potentially life-threatening condition requiring rapid treatment, and prompt radiological identification. Fortunately, MRI is usually able to convincingly make the diagnosis, distinguishing abscesses from other ring-enhancing lesions.
Epidemiology
Demographics reflect at-risk groups (see below) with all age groups being affected.
Risk factors
Risk factors for haematogenous spread include :
- right to left shunt
- congenital heart disease
- pulmonary AVM and AVFs as seen in hereditary hemorrhagic telangiectasia (HHT)
- infective endocarditis
- intravenous drug use (IVDU)
- lung infection
- sinonasal infections
- dental abscess
- systemic sepsis
Clinical presentation
Clinical presentation is non-specific, with many cases having no convincing inflammatory or septic symptoms. Symptoms of raised intracranial pressure, seizures and focal neurological deficits are the most common forms of presentation. Eventually, many abscesses rupture into the ventricular system, which results in a sudden and dramatic worsening of the clinical presentation and often heralds a poor outcome.
Pathology
Cerebral abscesses result from pathogens growing within the brain parenchyma. Initial parenchymal infection is known as cerebritis, which may progress into a cerebral abscess. Historically direct extension from sinus or scalp infections was the most common source. More recently hematological spread has become most common. Direct introduction by trauma or surgery accounts for only a small minority of cases .
Cerebral infection is commonly divided into four stages with distinct imaging and histopathologic features:
Microbiology
- Streptococcus sp: 35-50%
- especially S. pneumoniae
- sterile: 25%
- mixed: variable, 10-90% of cases depending on source
- Staphylococcus aureus and epidermidis: following neurosurgery
- Gram-negative species more common in infants
- Listeria in pregnant women and older patients
- group B Streptococcus (GBS) and E. coli in neonates
The immunocompromised patient is susceptible to a host of other organisms including :
- Toxoplasma gondii
- Nocardia asteroides
- Candida albicans
- Listeria monocytogenes
- Mycobacterium spp.
- Aspergillus fumigatus
Radiographic features
Both CT and MRI demonstrate similar features, although MRI has a greater ability to distinguish a cerebral abscess from other ring-enhancing lesions:
- a discrete lesion with a thin enhancing rim
- the rim may be less-well defined along the peripheral aspect of the lesion (away from ventricles)
- +/- additional "daughter" collections
- +/- ventricular extension, with accompanying ventriculitis
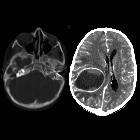
CT
In patients with suspected intraparenchymal sepsis, pre- and post-contrast scans should be obtained, unless the plan is to proceed to MRI regardless of the CT findings. Typical appearances include:
- outer hypodense and inner hyperdense rim (double rim sign) in most cases
- ring of iso- or hyperdense tissue, typically of uniform thickness
- central low attenuation (fluid/pus)
- surrounding low density (vasogenic edema)
- ventriculitis may be present, seen as enhancement of the ependyma
- obstructive hydrocephalus will commonly be seen when intraventricular spread has occurred
MRI
MRI is more sensitive than CT. Although peripherally-enhancing lesions may be non-specific by imaging, diffusion-weighted sequences (less commonly MR spectroscopy) showing central diffusion restriction are critical for suggesting the diagnosis of a cerebral abscess.
- T1
- central low intensity (hyperintense to CSF)
- peripheral low intensity (vasogenic edema)
- ring enhancement
- ventriculitis may be present, in which case hydrocephalus will commonly also be seen
- T2/FLAIR
- central high intensity (hypointense to CSF, does not attenuate on FLAIR)
- peripheral high intensity (vasogenic edema)
- the abscess capsule may be visible as an intermediate to slightly low signal thin rim
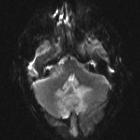
- DWI/ADC
- high DWI signal is usually present centrally
- represents true restricted diffusion.
- peripheral or patchy restricted diffusion may also be seen; this finding is however not as constant as one may think, with up to half of the rim-enhancing lesions demonstrating some restriction not proving to be abscesses.
- in some immunocompromised states, central content may not diffusion restrict
- SWI
- low-intensity rim
- complete in 75%
- smooth in 90%
- mostly overlaps with contrast-enhancing rim
- dual rim sign: a hyperintense line located inside the low-intensity rim
- low-intensity rim
- MR perfusion: rCBV is reduced in the surrounding edema cf. to both normal white matter and tumor edema seen in high-grade gliomas
- MR spectroscopy: elevated peaks are seen corresponding to lipids/lactate, succinate, acetate, and amino acids (alanine, valine, leucine, and isoleucine)
Treatment and prognosis
The mainstay of treatment for cerebral abscesses is neurosurgical intervention and drainage of the collection. This can be performed either by stereotactic aspiration or craniotomy . Broad-spectrum intravenous antibiotics are also needed and can later be changed to agents tailored to the specific organisms.
In cases where the abscess cavity does not completely obliterate, follow-up with MRI including DWI is useful and lack of restricted diffusion is reassuring. Demonstration of ongoing restricted diffusion in a cavity suggests persistent infection .
Differential diagnosis
The differential diagnosis typically includes other ring-enhancing lesions:
- metastasis or high-grade glioma (e.g. GBM)
- abscesses tend to have smoother inner wall
- satellite lesions favor infection
- abscesses may have low-intensity capsule
- rCBV elevated in high-grade gliomas, reduced in abscesses
- absent dual rim sign
- the cystic component does not show restricted diffusion, unlike abscess
- subacute infarction, subacute hemorrhage or contusion
- demyelinating lesion
- radiation necrosis
When a lesion demonstrates both ring enhancement and central restricted diffusion the differential is very much narrowed, and although cerebral abscess is by far the most likely diagnosis, the following should also be included on the differential :
- cerebral metastases: particularly necrotic adenocarcinoma
Siehe auch:
- Hirnmetastase
- Glioblastoma multiforme
- Sinusthrombose
- Metastase
- Demyelinisierende Erkrankung
- intrakranielle Echinokokkose
- Läsionen mit ringförmiger Kontrastmittelanreicherung
- septisch-embolische Herdenzephalitis
- cerebellar tuberculoma
- Strahlennekrose
- haemorrhage
- dermal sinus tract
- septisch-metastatische Herdenzephalitis
und weiter:
- zerebrale Verkalkungen
- subdurales Hygrom
- intrakranielle Verkalkungen
- Pilozytisches Astrozytom
- Neurozystizerkose
- Einklemmung
- Hirnödem
- Tuberkulose des ZNS
- Abszess
- Neurotoxoplasmose
- primäres ZNS-Lymphom
- neuroradiologisches Curriculum
- subdurales Empyem
- Kleinhirntumoren
- akute Otomastoiditis
- Gradenigo-Syndrom
- akute Sinusitis
- Ventrikulitis
- zerebrale Läsionen mit ringförmiger Kontrastmittelanreicherung
- bull's eye sign
- Tumefaktive Multiple Sklerose
- tumefaktive Demyelinisierung
- pott puffy tumour
- zystische Hirnmetastasen
- chronische Mittelohrentzündung
- Kleinhirnabszess
- zystische Hirntumoren
- intraaxial
- bakterieller Hirnabszess
- Tuberkulom des ZNS
- intrakranielle zystische Läsionen
- Hirnabszesse bei angeborenem Defekt der Sinus frontales
- cerebral abscesses secondary to contusions
- cystic lesion brain
- intrakranieller Abszess
- cerebellar abscess secondary to dermal sinus tract
- Pyramidenspitzen-Osteomyelitis
- brain abscess associated to Rendu-Osler-Weber disease
- MRI cerebellar abscess with spectroscopy
- Doppelrandzeichen Hirnabszess
- brain nocardiosis
- otogene Hirnabszesse
- bakterielle Enzephalitis
- diffusion MRI of brain abscess
- multiple cerebral abscess post head injury
- Hirnherniation

 Assoziationen und Differentialdiagnosen zu Kleinhirnabszess:
Assoziationen und Differentialdiagnosen zu Kleinhirnabszess:






