Hepatic fibrosis


























































Cirrhosis (rare plural: cirrhoses) is the common endpoint of a wide variety of chronic liver disease processes which cause hepatocellular necrosis. Cirrhosis can be diagnosed with ultrasound, CT, and MRI, and these imaging modalities can also be used to evaluate for possible complications of cirrhosis, such as portal hypertension or hepatocellular carcinoma.
Epidemiology
The demographics of cirrhosis reflect the underlying causes. Alcoholism and viral hepatitis from IV drug use or in an endemic region are the common causes.
The distribution of underlying etiology will vary regionally, with viral hepatitis being much higher in the developing world, especially Asia. A typical distribution of causality in Western nations is a follows :
- alcohol: 60-70%
- viral hepatitis: 10%
- hepatitis B virus most common in sub-Saharan Africa and Asia
- hepatitis C virus most common in the Western countries and Japan
- cryptogenic/non-alcoholic steatohepatitis (NASH): 10-15%
- biliary disease, e.g. primary sclerosing cholangitis (PSC), primary biliary cholangitis (PBC): 5-10%
- metabolic disease, e.g. hereditary hemochromatosis, Wilson disease, alpha-1-antitrypsin deficiency: 5%
- autoimmune hepatitis
- vascular disease, e.g. congestive hepatopathy (right heart failure), Budd-Chiari syndrome, hepatic veno-occlusive disease: rare
- cystic fibrosis: uncommon but increasing with increased survival
- medications (e.g. methotrexate)
Clinical presentation
The diagnosis is made either at screening for cirrhosis due to known risk factors, elevated liver enzymes, or discovered incidentally in an examination for non-specific symptoms (e.g. right upper quadrant pain). It may also present due to one of its complications:
Pathology
Focal hepatocellular necrosis caused by a variety of insults (see above) is accompanied by the three characteristics of cirrhosis :
Although traditionally cirrhosis has been divided into micro-and macronodular cirrhosis, many entities begin as micronodular (<3 mm) and progress to macronodular (e.g. alcoholic cirrhosis) and thus it is of limited utility as a classification scheme .
Severity scoring
- clinical scoring: Child-Pugh scoring system
- biochemical scoring: hepascore
- Metavir score
Radiographic features
Frequent findings in advanced cirrhosis include hypertrophy of the caudate lobe and lateral segments of the left lobe (segments 2 & 3) with concomitant atrophy of the posterior segments (6 & 7) of the right lobe. These changes are likely related to changes in blood flow between the segments. See article: caudate–right lobe ratio (C/RL).
Imaging is not reliable enough to differentiate between various underlying etiologies.
The main imaging challenge is distinguishing regenerative nodules, siderotic nodules and dysplastic nodules from:
- small HCC: early arterial enhancement with washout
- hepatic metastases: typically high T2
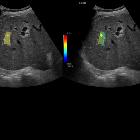
Ultrasound
Ultrasound is a major screening tool for cirrhosis and its complications. It is also useful to aid for biopsy. Appearances include:
- surface nodularity: (88% sensitive, 82-95% specific )
- overall coarse and heterogeneous echotexture
- segmental hypertrophy/atrophy (see above)
- caudate width: right lobe width >0.65 (43-84% sensitive, 100% specific )
- reduction of the transverse diameter (<30 mm) of the medial segment of the left lobe (segment 4)
- signs of portal hypertension
- Doppler flow changes
- portal venous system
- enlarged portal vein: >13 mm (42% sensitive, 95-100% specific )
- slow portal venous flow <15 cm/sec
- reversal or to-and-fro portal venous flow
- portal venous thrombosis +/- cavernous transformation
- enlarged SMV and splenic vein: >10 mm
- note: this should be measured during deep inspiration as size can vary.
- loss of respiratory variation in SMV and splenic vein spectral Doppler waveforms
- recanalization and hepatofugal paraumbilical (=umbilical) venous flow
- portosystemic collaterals
- hepatic veins
- portalisation of hepatic vein waveform
- hepatic arteries
- "corkscrew" appearance
- increased velocity (compensating for decreased portal vein flow)
- portal venous system
- splenomegaly
- ascites
- fatty change (variable)
- Doppler flow changes
Sonoelastography may also be useful to assess the amount of liver fibrosis . Suggested values for diagnosis
- >7 kPa: advanced fibrosis
- 12.5-15 kPa: cirrhosis
Contrast-enhanced ultrasound may have a role in the diagnosis of cirrhosis:
- diminished mean hepatic venous transit time is similar to that of perfusion CT .
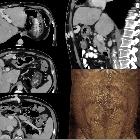
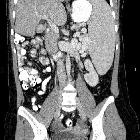
CT
CT is insensitive in early cirrhosis. More established findings include:
- surface and parenchymal nodularity
- regenerative nodules (majority): isodense/hyperdense to the rest of liver
- siderotic nodules (minority): hyperdense due to accumulation of iron
- fatty change (variable)
- parenchymal heterogeneity both on the pre and post IV contrast scans
- predominantly portal venous supply to dysplastic nodules.
- in advanced cirrhosis, nodular margin and lobar hypertrophy/atrophy may be demonstrated (see above).
- signs of portal hypertension
- portal vein enlargement
- portal venous thrombosis +/- cavernous transformation
- splenomegaly
- portosystemic collaterals
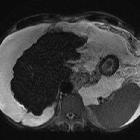
MRI
MRI is also insensitive in early cirrhosis but has a significant role in screening cirrhotic livers for small HCCs (see LI-RADS). MRI findings include:
- morphologic changes (same as on CT and ultrasound)
- regenerative nodules (or cirrhotic nodules)
- T1
- variable, usually isointense
- occasionally mildly hyperintense
- no early enhancement and washout as most supply is from the portal vein
- T2
- usually isointense
- hypointense if siderotic
- T1
- dysplastic nodules
- maybe of low or high grade, and thus have a variable appearance
- low-grade nodules will resemble regenerative nodules
- high-grade nodules will resemble HCCs
- small hepatocellular carcinoma (HCC)
- T1 C+ (Gd):
- arterial phase enhancement and washout
- late enhancing capsule
- growth in the interval between studies
- T2: typically mildly or moderately hyperintense
- T1 C+ (Gd):
MR angiography or a balanced steady-state free precession sequence may also be used to assess portal vein patency and portosystemic collaterals.
Treatment and prognosis
Treatment depends on the underlying etiology and presence of complications. One of the key roles of diagnostic radiology is the detection of hepatocellular carcinoma (six-monthly ultrasound should be done for surveillance as per 2018 AASLD (American Association for the Study of Liver Diseases) guidelines in cirrhotic patients to screen for HCC development) . Interventional radiology can be very helpful for the treatment of portal hypertension and its complications (e.g. TIPS, ascites drainage), as well as chemoembolisation or radiofrequency ablation of HCC.
Complications
- pulmonary: see pulmonary complications of cirrhosis
- MSK: see musculoskeletal complications of cirrhosis
- CNS: see CNS complications of cirrhosis
History and etymology
The word cirrhosis derives from the Ancient Greek word "κιρρόειν" ("to turn reddish-yellow" or "tawny"). Laennec was the first to use the term to describe the macroscopic appearance of fibrotic changes in a liver with alcoholic cirrhosis.
Differential diagnosis
There are several conditions that can potentially mimic cirrhosis on imaging :
- pseudocirrhosis
- widespread (miliary type) liver metastases
- Budd-Chiari syndrome-particularly chronic
- fulminant hepatic failure
- hepatic sarcoidosis
- congenital hepatic fibrosis
- idiopathic portal hypertension
- early primary biliary cholangitis (PBC)
- chronic portal vein thrombosis
- nodular regenerative hyperplasia of the liver
Practical points
- hepatopulmonary syndrome and hepatorenal syndrome may develop in cirrhosis
Siehe auch:
- Hypertrophie des Lobus caudatus
- hepatozelluläres Karzinom
- portosystemische Umgehungskreisläufe
- Lebermetastasen
- portale Hypertension
- Aszites
- Ösophagusvarizen
- Fundusvarizen
- Autoimmunhepatitis
- konfluierende hepatische Fibrose
- primär biliäre Cholangitis
- Budd-Chiari syndrome - particularly chronic
und weiter:
- kavernöse Transformation Pfortader
- Steatosis hepatis
- Regeneratknoten der Leber
- FNH
- fetthaltige Leberläsionen
- Splenomegalie
- arteriovenöse Malformationen der Lunge
- coarsened hepatic echotexture
- Alpha-1-Antitrypsin-Mangel
- zystische Fibrose
- renal papillary necrosis (mnemonic)
- asphyxierende Thoraxdysplasie (Jeune-Syndrom)
- Primär sklerosierende Cholangitis
- Caput medusae
- lipomatöse Impression der Vena cava inferior
- Caput medusae Zeichen bei DVA (developmental venous anomaly)
- Gynäkomastie
- noduläre regenerative Hyperplasie
- ADC abnormality of the basal ganglia
- Milzarterienaneurysma
- primary hepatic lymphoma
- sclerosing cholangitis
- altered alpha fetoprotein levels
- Hyperöstrogenismus
- Mammakarzinom beim Mann
- Cruveilhier-Baumgarten-Syndrom
- CA 125 elevation
- hyperechoic liver
- Lebertumoren
- adenomatöse Hyperplasie Leber
- Child-Pugh-Score
- hepatic hydrothorax
- differential diagnosis of diffuse gallbladder wall thickening
- papillary necrosis (mnemonic)
- Hepatopulmonales Syndrom
- milan criteria in liver tranplantation
- diffuse mesenteriale Flüssigkeitseinlagerungen (misty mesentery sign)
- generalised increased liver echogenicity
- hepatofugaler Fluss in der Vena portae
- Aflatoxin
- peribiliäre Zysten
- caudate-right lobe ratio
- contrast nephropathy
- abdominelle Manifestationen bei Mukoviszidose
- Pseudozirrhose der Leber
- peribiliary cysts in liver cirrhosis
- Teleangiektasie
- heterogenes Leberenhancement
- hepatobiliary manifestations of Wilson disease
- entzündliche Leberveränderungen
- abgerundeter Leberlappen

 Assoziationen und Differentialdiagnosen zu Leberzirrhose:
Assoziationen und Differentialdiagnosen zu Leberzirrhose: